
THE DIGESTIVE SYSTEM
DIGESTIVE PROCESS
Digestion is the
breaking down of larger food molecules into molecules small enough to be
absorbed by body cells. The organs that are
involved in this process make up the digestive system and include the alimentary
canal and its accessory organs. The activities of the digestive system entail
ingestion of food; secretion of about 9 liters/day of water, acid, buffers and
enzymes; mixing and propulsion of food along; digestion, either mechanical or
chemical (catabolic reactions) of food; absorption of end products of digestion
into blood or lymph vessels for distribution; and defecation or emptying of the
rectum.
The layers of the GI tract are the mucosa, submucosa, muscular, and serosa. The mucosa is the inner lining of the lumen and a mucous membrane. It has three layers: the epithelium (a protective layer of cells, the inner lining of GI tract), the lamina propria which contains blood, lymph nodes and vessels, and the muscular layer (a thin layer of smooth muscle). The submucosa layer contains blood vessels and connective tissue. A portion of the submucosal plexus controls secretions of GI tract. The muscularis layer contains some skeletal muscle at each end of GI tract but is mostly smooth muscle. There are two sheets of muscle fibers (circular and longitudinal). Involuntary contractions of the smooth musculature help breakdown food, mix it with digestive juices and propel (peristalsis) the food along. The myenteric plexus (of Auerbach) controls GI tract mobility. The serosa, outermost layer, is also called the visceral peritoneum (below the diaphragm).
The peritoneum is the largest serous membrane in the body. The parietal peritoneum lines the wall of the abdominal cavity whereas the visceral peritoneum covers some of the internal organs. The space between is the peritoneal cavity and it contains peritoneal fluid (ascites). The retroperitoneal organs are covered by peritoneum on the anterior surface only. The mesentery binds small intestine to the posterior abdominal wall. The mesocolon binds large intestine to posterior abdominal wall and carries blood and lymph vessels to the intestine. The falciform ligament attaches the liver to anterior wall and diaphragm. The lesser omentum suspends the stomach and duodenum from the liver and the greater omentum covers the transverse colon and coils of the small intestine. It also contains large quantities of fatty tissue and many lymph nodes.
Mouth (Oral or Buccal
cavity)
The structure of the mouth consists of the cheeks
(muscles on the side of the mouth), the lips (labia), a vermilion (transition
zone between lips and mouth), a labial frenulum (midline fold that attaches
inner surface of lips to gum), the vestibule (space between lips/cheeks and
gums/teeth), hard palate/soft palate (roof of mouth), the uvula (muscular
process hanging from soft palate), and tonsils (palatine and lingual). The
tongue is an accessory structure of digestive system. The musculature is
skeletal for voluntary action. Extrinsic muscles originate outside of the tongue
and insert into the tongue. Their function is side-to-side movement of food in
mouth. Intrinsic muscles originate inside tongue and they alter the shape and
size of the tongue to aid in speech and swallowing. A lingual frenulum limits
movement of tongue to the posterior. Teeth are accessory structures located in
the alveolar process of the jaw bones and are covered by the gums. The sockets
are lined by periodontal ligaments which anchor teeth into position and serves
as a shock absorber during chewing. The tooth consists of a crown, neck and
root. Dentin makes up most of the tooth and is covered by an enamel crown. The
pulp cavity lies in the crown of tooth and is filled with pulp (connective
tissue containing blood and lymph vessels. Humans have two sets of teeth; a
deciduous set consisting of twenty teeth and a permanent set of 32 teeth
Physiology of
digestion in the mouth
Mechanical chewing
(mastication) allows food to be mixed with saliva to form a bolus. From a
chemical point, salivary amylase initiates breakdown of starch and lingual
lipase digests triglycerides into fatty acids and monoglycerides. Swallowing
(deglutition) moves food from the mouth to the stomach by voluntary (mouth to
oropharynx) and involuntary (pharynx through esophagus to stomach) means.
Salivary glands
Most of work is done
by three pair of glands (parotid located beneath
and in front of ears), submandibular found beneath tongue, and sublingual which
are located superior to submandibular glands. Ducts from each gland carry saliva
to mouth. Saliva is 99.5% water, 0.5% sodium, potassium, chloride, bicarbonate
ions, phosphates and enzymes. Its function is based on the constituents: water
is medium for dissolving food; bicarbonates and phosphates buffer acidic foods;
chloride activates salivary amylase; and lysozyme kills bacteria. About 1000 -
1500 ml/day of saliva is secreted.
Esophagus
The esophagus contains
4 layers: mucosa, submucosa, muscularis and adventitia.
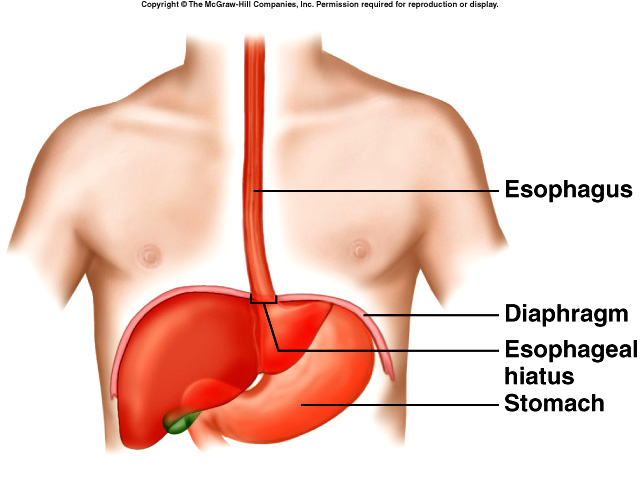 Cells
secrete mucous to aid in transport of food. The upper esophageal sphincter
relaxes to allow food to enter, peristalsis moves the food along the esophagus,
and the lower esophageal (gastroesophageal) sphincter relaxes and allows bolus
to enter the stomach. Achalasia occurs when the sphincter fails to relax
allowing food to remain in esophagus causing chest pains. Heart burn occurs when
the sphincter fails to close allowing stomach contents to irritate the
esophageal wall causing a burning sensation.
Cells
secrete mucous to aid in transport of food. The upper esophageal sphincter
relaxes to allow food to enter, peristalsis moves the food along the esophagus,
and the lower esophageal (gastroesophageal) sphincter relaxes and allows bolus
to enter the stomach. Achalasia occurs when the sphincter fails to relax
allowing food to remain in esophagus causing chest pains. Heart burn occurs when
the sphincter fails to close allowing stomach contents to irritate the
esophageal wall causing a burning sensation.
Stomach
The
stomach is a J-shaped enlargement of GI tract
located below diaphragm. It is composed of three muscle layers in muscularis.
Parts of the stomach are the cardia (surrounds the superior opening of the
stomach), the fundus (rounded area to left of cardia for food storage), the body
(main portion of stomach where mixing occurs), and the pylorus (attaches to
duodenum: pyloric antrum and canal). Rugae are folds in the mucosa of an empty
stomach. They allow the stomach to stretch. The pyloric sphincter is a valve
that connects stomach to small intestine.
The mucosa contains channels called gastric pits. Gastric glands at bottom of pits contain four types of secretory cells that secrete 2000-3000 ml of gastric juice per day. Chief cells secrete pepsinogen and gastric lipase. Parietal (oxyntic) cells secrete HCl and intrinsic factor. The mucous cells secrete mucous that protects the stomach wall. G-cells secrete gastrin into the blood.
Physiology of
Digestion in the stomach
Peristaltic movements called mixing waves mix
food with gastric secretions to form chyme. Chyme is moved forward and backward
in stomach to further mix. Some chyme is forced through pyloric sphincter but
some is left for more mixing. HCl denature proteins and stimulates secretion of
hormones that promote flow of bile and pancreatic juice. Enzymatic digestion of
proteins begins in stomach by pepsin. Amino acids are broken down into
peptides. Gastric lipase secreted by chief cells produce limited breakdown of
triglycerides.
Regulation of gastric secretions and motility is under control of nervous and hormonal mechanisms. In the cephalic phase, which is initiated by sensory receptors in brain, parasympathetic impulse promotes peristalsis and stimulate the gastric glands to secrete pepsinogen, HCl, and mucous into stomach and gastrin into blood. During the gastric phase, stretch receptors detect distention of stomach; chemoreceptors detect decreased pH of gastric juice which stimulate peristalsis and secretion of gastric juices. Peristalsis shoots 10-15 ml through pyloric sphincter. Gastrin secreted in pyloric region of stomach, is absorbed into blood where it travels to target cells (gastric glands) which secrete gastric juice.
Activation of the intestinal phase is due to receptors in the small intestine. Starting this phase inhibits mobility, preventing overloading of small intestine, and promotes continued digestion of food in stomach. It also triggers release of gastric inhibitory peptide (GIP), secretin and cholecystokinin (CCK). GIP stimulates secretion of insulin by pancreatic cells, inhibits secretion of gastric juices, and allows gastric emptying. Secretin stimulates secretion of pancreatic juice and bile rich bicarbonate ions. CCK stimulates secretion of pancreatic juice rich in digestive juices, causes ejection of bile from gallbladder, and induces satiety.
Emptying of the stomach is regulated by neural and hormonal reflexes. It is stimulated by distention of stomach and by gastrin and inhibited by GIP, CCK and enterogastric reflex of small intestine. Carbohydrates spend least amount of time in stomach, triglycerides spend the most. Absorption of some water, electrolytes, some drugs and alcohol occurs but the stomach is mostly impermeable to most substances.
Pancreas
The
pancreas is an accessory organ in the digestive
system as well as an important organ in the endocrine system. From a structural
point of view, the pancreas has a head, tail, body, and two ducts. The larger
duct is the pancreatic duct that joins the common bile duct to form the
hepatopancreatic duct which empties into the duodenum through the
hepatopancreatic ampulla. The smaller one is the accessory duct which also
empties into the duodenum. There are two cell types found in the pancreas. The
pancreatic islets secrete hormones (endocrine portion) and the acini (exocrine
portion) are enzyme secreting cells that secrete pancreatic juice.
Pancreatic juice contains enzymes that digest starch (pancreatic amylase), proteins (trypsin, chymotrypsin and carboxypeptidases), triglycerides (pancreatic lipase) and nucleic acids (ribo- and deoxyribonucleases). About 1200 - 1500 ml/day is produced. The pancreatic juice buffers the acidity of gastric juice making it slightly alkaline which prevents duodenal ulcers. Secretion of the juice is regulated by nervous and hormonal mechanisms. Exocrine secretions are necessary for normal digestion and absorption of dietary nutrients.
Liver
The
liver is the heaviest gland in the body. It
contains two lobes (the right lobe includes quadrate and caudate lobes). The
right and left lobes separated by falciform ligament. The liver is made up of
lobules which are the functional units of the liver. The lobules contain
hepatocytes (liver cells) arranged around a central vein. Kupffer’s cells are
reticuloendothelial cells that phagocytize worn out RBC/WBC. The liver possesses
sinusoids instead of capillaries. Hepatocytes produce bile which emulsifies
triglycerides during digestion.
About 800-1000 ml of bile is secreted daily. Bile is partially an excretory product and partially a digestive secretion (emulsifies fats). Nervous and hormonal factors regulate bile secretion. Bile flows via the right and left hepatic ducts that merge to form the common hepatic duct which merges with the cystic duct to form the common bile duct. Bile goes to the gallbladder via the cystic duct where it is stored. The common bile duct joins the pancreatic duct to form hepatopancreatic ampulla.
About 1400 ml of blood passes through the liver each minute (1000 ml from portal circulation). The vascular function of liver is storage and filtration.
Functions of the liver
-
Carbohydrate metabolism maintains normal glucose levels by storing glucose as glycogen when blood glucose levels are high and breakdown of glycogen to glucose when blood glucose is low.
-
Lipid metabolism stores triglycerides, breaks down fatty acids, synthesizes cholesterol and uses it to make bile salts.
-
Protein metabolism is a very important function. The liver deaminates amino groups to be used for ATP production, converts ammonia to urea for excretion, synthesizes plasma proteins such as fibrinogen and prothrombin, and performs transamination which converts one amino acid into another which may be needed by the body.
-
Removal of drugs and hormones by detoxification.
-
Excretion of bile.
-
Synthesis of bile salts that used to emulsify and absorb fats.
-
Storage of certain vitamins and minerals.
-
Phagocytosis of worn out RBC, WBC, and bacteria.
-
Activation of Vitamin D.
Gallbladder
The function of the
gallbladder is to store and concentrate bile.
When bile is needed in the small intestine, bile is forced into the cystic duct,
through the common bile duct, through the hepatopancreatic ampulla and into the
duodenum.
Small Intestine
Most of digestion and
absorption occurs in the small intestine.
Structurally the SI consists of three segments: duodenum about 10” long,
starts at the pyloric sphincter; jejunum about 8’ long; and ileum about 12’
long, joins the large intestine at the ileocecal sphincter. The mucosa contains
many cavities lined with glandular epithelium. Intestinal glands secrete
intestinal juice. The submucosa of duodenum contains duodenal (Brunner’s) glands
which secrete alkaline mucous that helps neutralize gastric acid. Villi are
finger-like projections on the mucosa. The core of the villi is the lamina
propria (a connective tissue layer containing an arteriole, a vein, a capillary
network, and a lacteal). Microvilli are found on the apical surface of the villi
and function as the brush border which increases the surface area for
absorption. The circular fold is a permanent ridge in the mucosa that enhance
the chyme to spiral rather than move in a straight line. Villi, microvilli, and
circular fold provide a large surface area for absorption. Two layers of muscles
form the muscularis. Solitary lymphatic nodules found in the lower ileum and
aggregated lymphatic follicles (Pyer’s patches) prevent bacteria from entering
the bloodstream.
Intestinal Juice and
Brush Border Enzymes
One to two liters of
intestinal juice (pH 7.6)
are secreted per day.
Pandreatic juice aids in the absorption of chyme. Brush border enzymes found in
the plasma membrane of the microvilli aid in digestion. Carbohydrate digesting
enzymes include a-dextranase,
maltase, sucrase, and lactase. Protein digesting enzymes include peptidases.
Nucleotide digesting hormones include nucleosidases and phosphatases.
Physiology of digestion
and absorption in the small intestine
Segmentation is the mixing of the contents of the small intestine and the
major movement of SI. Segmentation involves localized contractions in areas
containing food and mixes chyme with digestive juices and brings substance in
contact with the mucosa. Peristalsis propels the chyme along. Absorption is the
passage of the end products of digestion into blood or lymph vessels.
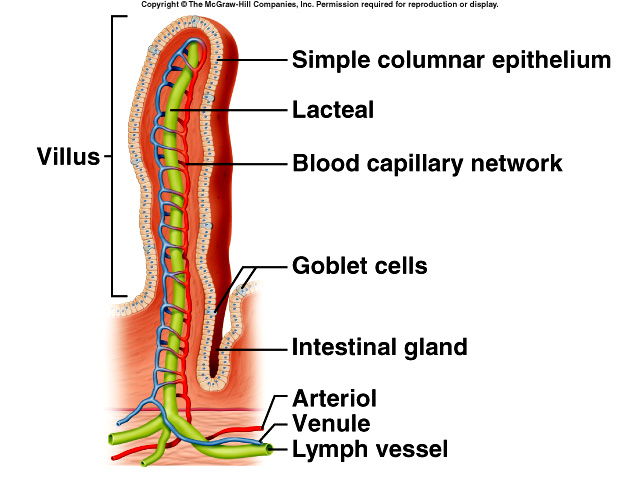 Ninety
percent of all absorption occurs in SI.
Absorption
occurs by diffusion, facilitated diffusion, osmosis, and active transport are
mechanisms. Monosaccharides utilize facilitated diffusion and active transport;
proteins are broken down into amino acids and absorbed by active transport, and
short chain fatty acids pass into the blood stream by simple diffusion. Long
chain fatty acids are absorbed as part of micells (tiny spheres) and then
re-synthesized into triglycerides and formed into chylomicrons. The
chylomicrons move into lymph in the lacteal of a
villus and are carried in the blood at the R/L lymphatic ducts as a lipoprotein.
The SI absorbs water, electrolytes and vitamins. About 9 liters pass into SI of
which about 8 are reabsorbed.
Ninety
percent of all absorption occurs in SI.
Absorption
occurs by diffusion, facilitated diffusion, osmosis, and active transport are
mechanisms. Monosaccharides utilize facilitated diffusion and active transport;
proteins are broken down into amino acids and absorbed by active transport, and
short chain fatty acids pass into the blood stream by simple diffusion. Long
chain fatty acids are absorbed as part of micells (tiny spheres) and then
re-synthesized into triglycerides and formed into chylomicrons. The
chylomicrons move into lymph in the lacteal of a
villus and are carried in the blood at the R/L lymphatic ducts as a lipoprotein.
The SI absorbs water, electrolytes and vitamins. About 9 liters pass into SI of
which about 8 are reabsorbed.
Large Intestine
The functions of the
LI is the completion of absorption, manufacture certain vitamins, and formation
and expulsion of fecal material. Structurally the LI is attached to the
abdominal wall by the mesocolon and attached to the small intestine at the
ileocecal sphincter. It is about 5’ long consisting of the cecum, colon, rectum,
and anal canal. The cecum is a pouch below the ileocecal valve. The vermiform
appendix is attached to lower cecum. The colon
consists of ascending, transverse, descending, and sigmoid portions. Bends are
the right colic (hepatic) flexure and left colic (splenic) flexure. The rectum
is inferior to the sigmoid colon followed by the anal canal and anus. Teniae
coli is a muscularis that consists of longitudinal muscles which are thickened
and gather the colon into series of pouches called haustra. Epiploic appendages
are small pouches filled with fat and attached to Teniae coli.
Physiology of
digestion in LI
Mechanical movements
include haustral churning, peristalsis, and mass peristalsis. Haustra remain
relaxed until they fill, then squeeze contents into next haustra. Mass
peristalsis occurs about 4 times per day after eating and is called a
gastrocolic reflex because food in stomach initiates reflex. The last stages of
chemical digestion occur through activity of bacteria. Absorption water,
electrolytes and vitamins occurs. The remainder of what is left becomes feces
and includes water, inorganic salts, epithelial cells, bacteria and undigested
food.
Defecation is the elimination of feces from the rectum. It is a reflex action is aided by voluntary contractions of the diaphragm and abdominal muscles and relaxation of the anal sphincter.
THE URINARY SYSTEM
In chapter four, Cellular Metabolism, we saw that cells produce waste products (CO2, H2O, NH4, urea and heat). In addition to these, certain ions build up in the system. All of these toxic waste products and excess ions must be excreted from the body. The organs that eliminate waste products are:
-
Kidneys: excrete H2O, NH4, urea, some toxins, some electrolytes (excess ions), heat and CO2.
-
Lungs: excrete CO2, heat, and some H2O.
-
Skin: excrete heat, H2O, CO2 and small amount of salts.
-
GI tract: solid, undigested food is eliminated, excretes CO2, water and heat.
The primary function of the urinary system is to help maintain homeostasis by controlling the composition, volume and pressure of blood. The threat to life in renal failure often comes not from the accumulation of metabolic wastes, but from loss of the body's ability to balance the daily intake of salts and water with the appropriate rate of excretion.
The Kidneys
 The
functions of the kidneys are to remove wastes from blood as urine, control blood
pH by excreting excess H+, and to regulate blood pressure by
excreting renin. Metabolism functions of the kidneys include gluconeogenesis
(synthesize glucose), secretion of erythropoietin which stimulates RBC formation
and participation in the synthesis of Vitamin D.
The
functions of the kidneys are to remove wastes from blood as urine, control blood
pH by excreting excess H+, and to regulate blood pressure by
excreting renin. Metabolism functions of the kidneys include gluconeogenesis
(synthesize glucose), secretion of erythropoietin which stimulates RBC formation
and participation in the synthesis of Vitamin D.
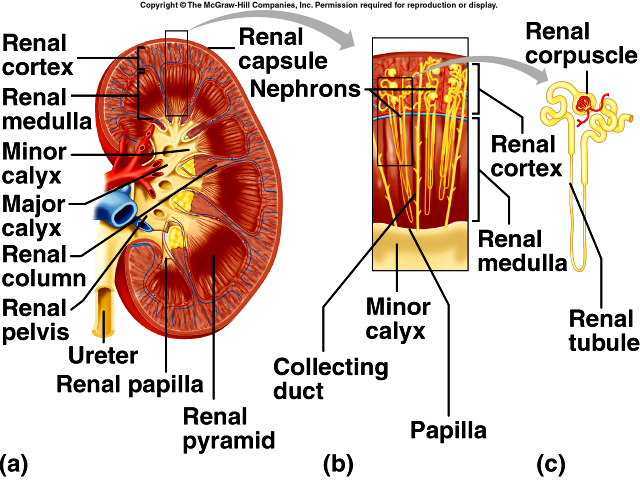
The kidneys are shaped like a pair of large kidney beans weighing @125-250 gm each. A hilum, a notch in center of one of the sides, allows blood and lymph vessels and the ureter to enter and/or leave the kidney. External to the kidney are a series of layers. The renal capsule is the innermost layer followed by the adipose capsule and renal fascia. Their function is to protect the kidney against trauma and to anchor the kidney to the abdominal wall.
The kidney can be divided into an outer region, the cortex, and an inner region, the medulla. There are 8-18 renal pyramids found in the medulla. Their bases face the cortex and their apexes are called renal papillae. Renal columns are portions of the cortex that extend between the renal pyramids. The renal pelvis is a cavity into which urine drains. Each kidney contains 2-3 major calyces along with the 8-18 minor calyces. Urine drains from the pyramids into the minor calyces, which drain into the major calyces to the renal pelvis and out via the ureter.
Blood Flow
through the Kidneys
The Renal arteries branch into five segmented arteries which branch into
interlobar arteries (found in the renal columns) which branch into arcuate
arteries (base of the renal pyramids) which branch into interlobular arteries
that branch into an afferent arterioles (in cortex) for each nephron and then
into the glomerular capillaries (glomerulus). The glomerular capillaries then
unite to form the efferent arterioles which divide to form the peritubular
capillaries and/or vasa recta (juxtamedullary
nephrons only). Eventually the peritubular capillaries unite to form the
interlobular veins which unite to form the arcuate veins that unite to
form the
interlobar veins that unite into the segmental veins that
unite into the renal veins. About 20-25% of blood passes through the kidneys
every minute.
The nephron is the functional unit of
the kidney. Its function is to produce urine by filtration, secretion and
reabsorption.
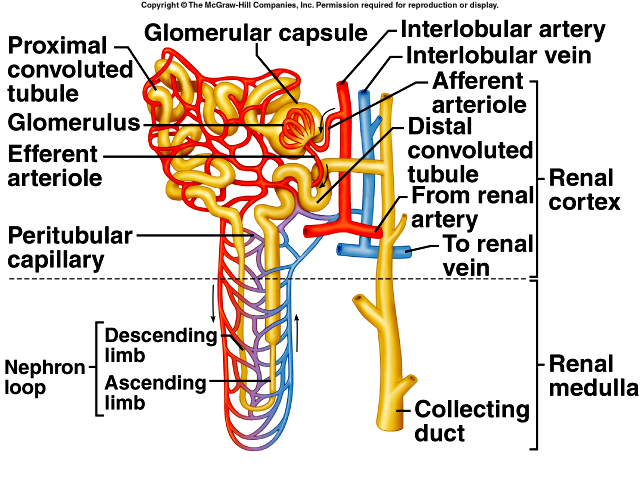 The
parts of the nephron include a renal corpuscle (fluid is filtered here) and a
renal tubule (filtered fluid passes into this structure). The renal
corpuscle is composed of a glomerulus (tuft of capillaries that lies within) and
the glomerular capsule (Bowman's capsule). Blood
enters the renal corpuscle through afferent arterioles and exits through
efferent arterioles. Inside the capsule, water and solutes are filtered from
blood and pass through the proximal convoluted tubule to the nephron loop
(descending limb and ascending limb) to the distal convoluted tubule.
Several distal convoluted tubules are linked to form a
single collecting duct. Several collecting ducts merge to form papillary ducts
which drain into a minor calyx. There are about 30 papillary ducts per renal
papillae. The
renal capsule and convoluted tubules lie in the cortex whereas the nephron loop
is found in the medulla.
The
parts of the nephron include a renal corpuscle (fluid is filtered here) and a
renal tubule (filtered fluid passes into this structure). The renal
corpuscle is composed of a glomerulus (tuft of capillaries that lies within) and
the glomerular capsule (Bowman's capsule). Blood
enters the renal corpuscle through afferent arterioles and exits through
efferent arterioles. Inside the capsule, water and solutes are filtered from
blood and pass through the proximal convoluted tubule to the nephron loop
(descending limb and ascending limb) to the distal convoluted tubule.
Several distal convoluted tubules are linked to form a
single collecting duct. Several collecting ducts merge to form papillary ducts
which drain into a minor calyx. There are about 30 papillary ducts per renal
papillae. The
renal capsule and convoluted tubules lie in the cortex whereas the nephron loop
is found in the medulla.
Cortical and juxtamedullary nephrons are the two types of nephrons. The cortical nephron has its glomerulus located in the outer and mid regions of the cortex of the kidney; its short nephron loop just penetrates the medulla.
The glomerulus of the juxtamedullary nephron is placed in the inner region of the cortex and the long nephron loop that almost reaches the renal papillae is in the medulla: 15-20% of the nephrons have the long loop. The Juxtaglomerular apparatus (JGA) consists of juxtaglomerular cells of the afferent arteriole and the macula densa (tall epithelial cells) of the distal convoluted tubule. The JGA helps regulate blood pressure and the rate of filtration in the kidneys by release of the hormone renin from cells located in the afferent arteriole.
Physiology of Urine Formation
The nephrons do the work in the kidneys. They control blood concentration and
volume by removing selected amounts of water and solutes, regulate pH by
removing excess H+ and remove toxic wastes from the blood (creatinine,
urea, urates). They do
this by glomerular filtration, tubular secretion
and tubular reabsorption.
In glomerular filtration about 180 l/day of filtrate (plasma is filtered through the glomerular capillaries) is passed through the membranes. The glomerular capillaries are long, providing a large surface area for filtration and the endothelial-capsular membrane is thin allowing for a greater filtration rate. Capillary BP is higher in the glomerulus due to smaller size of the efferent arteriole and this translates in a greater amount of filtrate.
Net filtration pressure (NFP): NFP = GCHP - (CHP + GCOP)
The filtration of blood depends on three mechanisms; glomerular capillary hydrostatic pressure (GCHP) minus the capsular hydrostatic pressure (CHP) and the glomerular capillary osmotic pressure (GCOP). CHP & GCOP oppose GCHP and push blood back into capillary.
Glomerular Filtration Rate (GFR) is the amount of filtrate that forms every minute (about 125 ml/minute or 180 l/day). Factors that affect the NFP will alter the GFR. For example, anuria occurs when the daily output of urine <50 ml. Homeostasis requires a constant GFR. If GFR too high, the system may lose needed substances. If GFR too low, it may cause a buildup of toxic waste products. GFR tends to decrease with age and in renal disease due to a decrease in the number of functioning glomeruli. Measurement of GFR is an important index of renal function and progression or amelioration of renal disease.
Regulation of GFR
Glomerular blood flow depends on auto regulation,
hormonal regulation and neural regulation. GFR remains relatively constant
due to auto regulation but can decrease by strong stimuli from renal nerves.
Auto regulation enables the kidneys to maintain a constant BP & GFR and this
occurs within the kidneys. Hormonal regulation is due to angiotensin II, atrial
natriuretic peptide (ANP), and aldosterone. Renin is secreted by JGA into the
blood and converts angiotensinogen into angiotensin I which is further converted
to angiotensin II in the lungs. Angiotensin II causes vasoconstriction of
efferent arterioles raising glomerular BP & GFR. It also stimulates secretion of
aldosterone by adrenal cortex, which enhances reabsorption of sodium and water,
stimulates thirst center in hypothalamus, and stimulates release of antidiuretic
hormone (ADH) by pituitary gland which results in water retention.
Atrial Natriuretic Peptide (ANP) is secreted by the stimulation of the heart and promotes the excretion of water and sodium which causes an increase of GFR. ANP also suppresses secretion of ADH, aldosterone and renin.
Tubular Reabsorption is the movement of filtrate back into peritubular capillaries or vasa recta. About 99% of the filtrate is reabsorbed as it passes through the tubules. There are microvilli present on the apical surfaces of cells lining the lumen that function in reabsorption. Glucose, amino acids, ions, water and nutrients are reabsorbed. Reabsorption of sodium occurs in the proximal convoluted tubule (PCT). The amount of sodium reabsorbed is second only to amount of H2O reabsorbed and is done by active transport. When sodium is actively transported, it promotes the passive diffusion of other solutes and water that travel with the sodium. ATP is used as energy source. Almost 100% of filtered glucose, amino acids, lactic acid and other metabolites are reabsorbed in the PCT. This is done by a method called secondary active transport and uses cellular structures called symporters. There is a transport maximum; a limited amount of a substance that can be absorbed. At the renal threshold, if the plasma concentration of the substance is exceeded and the excess nutrients spill into the urine. This happens in diabetes because blood glucose levels are high due to insulin deficiency and as a result glucose spills over into the urine (glucosuria). Eighty to ninety percent of HCO3-, 65% of sodium and H2O, 50% of Cl- and K+ are absorbed in the PCT.
Reabsorption in Nephron Loop
Forty percent of K+, 25% of Na+ of Cl- and 15%
of H2O are reabsorbed in the nephron loop. Here again symporters are used to
bring these ions across membranes.
Reabsorption in the DCT and
Collecting Tubules
About 95% of the filtrate has already been reabsorbed by the time it gets to the
DCT. Aldosterone and ADH act on principle cells in DCT to regulate final
concentrations that have to be reabsorbed. If ADH is absent about 20 liters of
dilute urine is excreted/day. If ADH is at maximum levels, then only 400-500
ml/day are excreted. Normally is 1-2 liters of urine is excreted per day. About
90% of water has already been reclaimed. The last 10% occurs in collecting
tubules due to ADH.
Renal clearance refers to the ability of kidneys to remove
(clear) substance from filtrate.
Tubular Secretion
The purpose of tubular secretion is to rid the body of certain materials and
control pH. Secretion of K+ is important, because if K+ is
not secreted, cardiac arrhythmia may develop which can lead to death. It is
controlled by aldosterone, the K+ concentration in the plasma and the
Na+ concentration in the DCT. The
secretion
of H+ requires a high energy active transport process. Blood pH can
be maintained in 3 ways: secrete H+ ions into the filtrate,
reabsorbing filtered HCO3- , and by processing new HCO3-.
This takes place
in the epithelial cells of the PCT where antiporters (counter transporters are
used) and in the collecting ducts. Most HCO3- combines
with H+ to form H2CO3 which disassociates into CO2 and water. Secretion
of urea and ammonia is necessary because ammonia is toxic to the body.
Antiporters are used to secrete and the amount secreted is dependent on blood
pH.
Evaluation of Kidney Function
Laboratory tests used include BUN (Blood Urea Nitrogen) which measures the
nitrogen that is part of urea. When GFR decreases due to renal disease or
obstruction, BUN increases. The plasma
creatinine measures how efficiently a substance is removed. High renal clearance
equals efficient removal. The renal
plasma clearance test depends on filtration, reabsorption and secretion.
Producing dilute and concentrated urine is dependent on ADH. In the mechanism of urine dilution, urine must contain more water than that found in blood. It must be hypotonic to plasma. This is due to renal tubules absorbing more solutes than water. In the mechanism of urine concentration, more water is reabsorbed in the tubules (done to conserve water, yet eliminate wastes). Urine must be hypertonic to plasma. The mechanisms involve differences in solute and water reabsorption in different sections of the nephron loop and the collecting ducts. In the nephron loop, Na+, K+, and Cl- are reabsorbed from filtrate into interstitial fluid of the medulla and pass into the vasa recta. In the collecting duct increase ADH and more water will be absorbed, thus concentrating the urine. Urea recycling is affected by presence of ADH. Water absorbed in collecting duct causes urea to buildup in interstitial fluid. Urea passes into the filtrate and is passed in the urine. The counter current mechanism is based on the location of the juxtamedullary nephrons and the vasa recta. Urine becomes more concentrated as it flows down the descending limb and more dilute as it moves up the ascending limb.
Hemodialysis is used when kidneys cannot function by themselves and it is performed to mechanically cleanse blood. This is done about three times per week by continuous ambulatory peritoneal dialysis, which can be done at home and is easier than hemodialysis but has more risk of infection.
Urine
1000-2000 ml/day of urine is produced. Volume can be influenced by diuretic and
antidiuretic drugs. Urochrome gives it a pale to yellow pigment. The darker the
color the more concentrated it is. Urine can also be red, green, blue, brown, or
black due to diet or disease. Usually urine is clear but can be cloudy due to
the presence of mucous, cells, or salts (phosphates, urates). Urine develops an
ammonia smell upon standing and the urine of diabetics has a sweet odor due to
ketone bodies. The range of pH
4.6 - 8.0, usually about 6.0 and the specific gravity is 1.001 - 1.035.
Abnormal constituents in urine can include:
-
Albumin (albuminuria): most common protein found in urine
-
Glucose (glucosuria): indicates diabetes
-
RBC (hematuria): indicates disease of some type
-
WBC (pyuria): indicates infection in the kidneys or urinary organs
-
Ketone bodies (ketosis): indicates diabetes
-
Bilirubin (bilirubinuria) and urobilinogen (urobilinogenuria): indicates breakdown of RBC and hemoglobin
-
Casts: tiny masses of material in the shape of lumen (WBC, RBC, epithelial casts)
-
Microbes: bacteria, yeast, protozoa
Other Urinary Tract Structures
Two ureters, one from each kidney, connect each kidney from the renal pelvis to
the bladder. There are three layers in the walls of the ureters. A muscularis
layer functions in moving urine from kidney to bladder by peristalsis. It is in
the ureters that renal calculi (kidney stones) most often will lodge. If the
obstruction is not removed, the kidney will fail. Lithotripsy or surgery is used
to remove it.
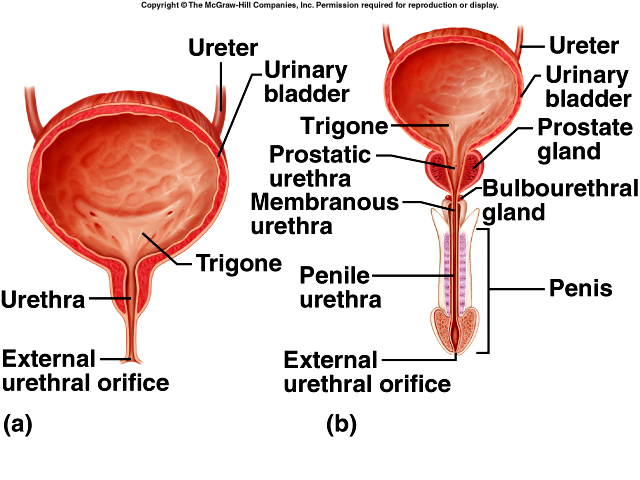 The
urinary bladder
is a hollow organ used to store urine. It is located anterior to rectum in the
male and anterior to the vagina and inferior to the uterus in the female which
causes it to be smaller. The trigone is a triangular area in the base of the
bladder bounded by two ureteral openings and the internal urethral orifice
(opening to the urethra). Rugae
allow the bladder to stretch. The detrusor muscle is three layers of muscle in
the walls of the bladder. An internal urethral sphincter is a muscle found
around the opening to the urethra. The external urethra sphincter is used for
voluntary control of urination.
The
urinary bladder
is a hollow organ used to store urine. It is located anterior to rectum in the
male and anterior to the vagina and inferior to the uterus in the female which
causes it to be smaller. The trigone is a triangular area in the base of the
bladder bounded by two ureteral openings and the internal urethral orifice
(opening to the urethra). Rugae
allow the bladder to stretch. The detrusor muscle is three layers of muscle in
the walls of the bladder. An internal urethral sphincter is a muscle found
around the opening to the urethra. The external urethra sphincter is used for
voluntary control of urination.
Urination or micturition allows urine to leave the bladder. The urge to urinate impulses is sent when the bladder is 1/4 to 1/2 full. An automatic bladder refers to cases where there are no sensory stimuli from higher nervous center (spinal cord injuries) the bladder can fill and empty spontaneously. Initially there is a reflex due to stimuli but the reflex can be controlled through the external urethral sphincter. Problems with urination range from incontinence or the lack of voluntary control to retention (incomplete voiding) and are often due to an obstruction in the urethra.
The urethra is a tube leading from bladder to the exterior urethral orifice. Its function is to carry urine out of the body.
REPRODUCTIVE SYSTEM
Reproduction is the process by which a species continues to survive. Genetic material is passed from one generation to the next. The reproductive organs are called gonads because they produce gametes (sperm cells in the male and ova in the female). Gonads also produce hormones. Also involved in the reproductive system are the ducts, which transport and store the gametes, and the accessory sex glands, which produce materials that support the gametes.
Male Reproductive System
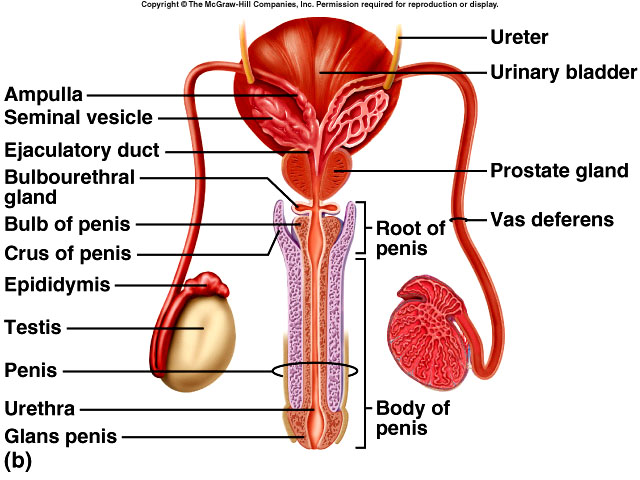 The
testes (testicles) are a pair of oval glands
located in the scrotum. They contain seminiferous tubules that produce sperm
cells, sustentacular (Sertoli) cells that support, protect, and nourish sperm
cells and secrete inhibin (a hormone that helps regulate sperm production by
inhibiting FSH), and interstitial cells (cells of Leydig) which secrete
testosterone. The testes are divided into 200-300 compartments called lobules by
the tunica albuginea. Each tubule contains 1-3 seminiferous tubules.
The
testes (testicles) are a pair of oval glands
located in the scrotum. They contain seminiferous tubules that produce sperm
cells, sustentacular (Sertoli) cells that support, protect, and nourish sperm
cells and secrete inhibin (a hormone that helps regulate sperm production by
inhibiting FSH), and interstitial cells (cells of Leydig) which secrete
testosterone. The testes are divided into 200-300 compartments called lobules by
the tunica albuginea. Each tubule contains 1-3 seminiferous tubules.
Spermatogenesis is an ongoing process by which sperm are made and the chromosome number is reduced to (n) or the haploid number of chromosomes. Humans have 23 pairs or 46 chromosomes. Twenty-two pairs are homologous and are called autosomes. One pair (XY) is called the sex chromosomes and this chromosome determines the sex of the individual. Meiosis is the process by which the gametes produced receive the haploid number of chromosomes. Spermatogonia line the seminiferous tubules and contain 2n chromosomes (46 in humans). Spermatogonia differentiate into primary spermatocytes (2n) which then undergo two successive nuclear divisions (Meiosis I). In the chromosomes the DNA replicates and the 46 chromosomes move to the equatorial plane of the cell where they line up in pairs (synapses). Tetrad formation occurs enabling crossing over of genetic material on the chromatids. The result is 2 secondary spermatocytes (n) but each chromosome is still made up of 2 chromatids attached by a centromere. The second equatorial division (Meiosis II) takes place. The chromatids separate and each spermatid formed have 23 chromosomes. Each primary spermatocyte produces four spermatids.
Spermiogenesis involves the maturation of the spermatid into spermatozoa. The function of spermatozoa is to fertilize an oocyte. About 300 million spermatozoa mature each day. They can survive in the female reproductive tract for up to 48 hours. A mature sperm consists of a head (nucleus and acrosome: hyaluronidase and proteinase that aid in the penetration of the oocyte), a midpiece (containing mitochondria which produce energy for locomotion), and a tail.
Hormones
of the Brian-Testicular Axis
At puberty, gonadatropin-releasing hormone (GnRH) stimulates the pituitary gland
to secrete FSH and LH (luteinizing hormone). FSH initiates the spermatogenesis
and LH assists in spermatogenesis and stimulates testosterone production. In the
male LH is often called interstitial cell stimulating hormone (ICSH).
Testosterone is an androgen. It controls the growth, development, and
maintenance of the sex organs. In the male it stimulates bone growth, protein
anabolism, and sperm maturation. In addition it also stimulates development of
male secondary sex characteristics and contributes to male sexual behavior and
to the sex drive in both males and females. Inhibin is a protein hormone
secreted by the sustentacular cells that inhibits FSH thus helping to regulate
the rate of spermatogenesis.
Ducts
The duct system in the testes includes the seminiferous tubules, straight
tubules and the Rete testis. Sperm leave the testes through efferent ducts and
pass into the ductus epididymis (a twenty foot long duct) where sperm are stored
and mature (become motile and fertile) for 10-14 days. Sperm can remain in the
epididymis for @ a month after which they are expelled or reabsorbed.
The ductus (vas) deferens stores sperm or moves sperm from the epididymis to the urethra. During a vasectomy a portion of the vas deferens is removed and the ends are tied. The vas deferens terminates at the ampulla of the ductus deferens. Ejaculatory ducts are found in the union of the duct from the seminal vesicle and the ductus deferens. They eject sperm into the prostatic urethra. The urethra serves as a passageway for both semen and urine and is composed of the prostatic urethra, the membranous urethra, and the spongy penile urethra.
Accessory sex glands secrete most of the fluid portion (seminal fluid) of semen. Seminal vesicles are a pair of glands that secrete an alkaline viscous component of the fluid. The seminal vesicles contribute about 60% of seminal fluid. Alkalinity of the fluid neutralizes the acidity of the female genital tract. Fructose in the fluid provides energy for the sperm. Prostaglandins contribute to sperm’s motility and viability and fibrinogen causes semen to coagulate after ejaculation (affords a protection for sperm while in the vagina. The prostrate gland secretes a thin milky-like, slightly alkaline fluid (33% of fluid volume). Clotting enzymes activate fibrinogen and fibrinolysin breaks down the clot. The prostate gland may enlarge after 45 years old. A pair of bulbourethral glands secretes an alkaline substance that protects semen from acids in the urethra.
Semen is a mixture of spermatozoa and fluids from the accessory glands. Secretions provide fluid for movement, nutrients, and they neutralize the acid environment of the male urethra and the female genital tract. The average volume is 2.5-5cc with @ 50-150 million sperm per milliliter. If a male produces <20 million/ml, it means he is probably sterile. Semen contains an antimicrobial seminal plasmin that can destroy certain bacteria. Semen analysis checks for volume, mobility, count, liquefaction, morphology, pH, fructose; it is always done in cases of infertility and after vasectomy.
The scrotum is an out pouching of skin that supports the testes. It is located outside to body proper because sperm will die at the higher temperature inside of the body. The cremaster muscle elevates the testes during sexual arousal and on exposure to cold and relaxation of the moves the testes away from the body. In this way it regulates the temperature of the testes. The dartos muscle gives the scrotum a wrinkled appearance.
The function of the
penis is to introduce spermatozoa into the vagina
and to convey urine to outside of the body. Parts of the penis include a pair of
erectile tissues called the corpora cavernosa and corpus spongiosum (contains
spongy urethra) contain sinus tracts for blood. The root of the penis consists
of the bulb, crura and the base of the corpus spongiosum. The distal end
contains the glans penis, corona, external urethral orifice. Covering the glans
penis is the prepuce or foreskin which may be removed.
Female Reproductive Organs
The ovaries are a pair of glands homologous to the testes. They are supported in
the body by a broad ligament that anchors the
uterus to either side of the parietal peritoneum, the mesovarium, which is part
of the peritoneum and attaches the ovaries to the broad ligament, the ovarian
ligament, that anchors the ovaries to the uterus, and the suspensory ligament
that anchors the ovaries to the pelvic wall. Germinal epithelium covers the
ovaries. The tunica albuginea is connective tissue immediately below the
germinal epithelium. Ovarian follicles consist of oocytes at various
stages of development. A vesicular ovarian (Graafian) follicle is a large fluid
filled follicle that contains an immature ovum. Its function is to secrete
estrogen. The corpus luteum is a mature vesicular ovarian follicle that has
released its oocyte (ovulation). It produces progesterone, estrogens, inhibin,
and relaxin before degenerating into the corpus albicans. The functions of the
ovaries are to produce and discharge a secondary oocyte and to secrete hormones.
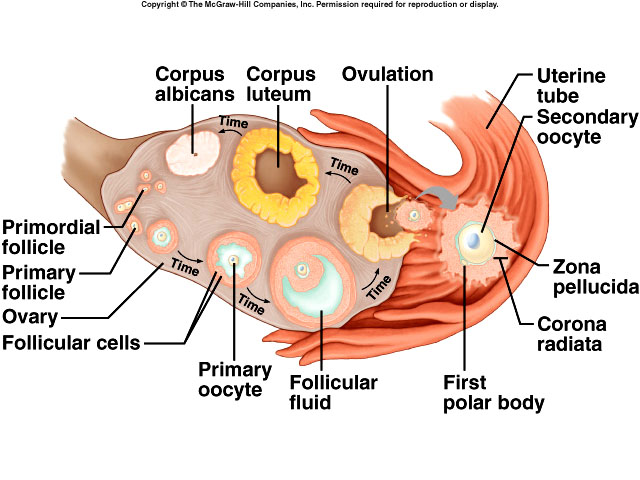 Oogenesis
is the formation of a haploid ovum. In reduction division (Meiosis I), the
oogonium develops into a primary oocyte (2n) during prenatal development. These
do not complete meiosis until after the female reaches puberty. The primordial
follicle is a primary oocyte surrounded by epithelial cells. One to two million
primordial follicles are present at birth. Most degenerate till there are
40-400K at puberty. Each month after puberty, FSH causes @20 primordial
follicles to become primary follicles. Most degenerate but one primary oocyte
undergoes meiosis which results in a secondary oocyte and a first polar body,
each having (n) chromosomes. The secondary oocyte gets most of the cytoplasm, is
surrounded by granulosa cells and the structure is now called a secondary
follicle. The secondary oocyte starts Meiosis II producing another polar body
and a larger cell that develops into an ovum. Meiosis II is completed after
fertilization. The first polar body can also divide producing two more polar
bodies that disintegrate.
Oogenesis
is the formation of a haploid ovum. In reduction division (Meiosis I), the
oogonium develops into a primary oocyte (2n) during prenatal development. These
do not complete meiosis until after the female reaches puberty. The primordial
follicle is a primary oocyte surrounded by epithelial cells. One to two million
primordial follicles are present at birth. Most degenerate till there are
40-400K at puberty. Each month after puberty, FSH causes @20 primordial
follicles to become primary follicles. Most degenerate but one primary oocyte
undergoes meiosis which results in a secondary oocyte and a first polar body,
each having (n) chromosomes. The secondary oocyte gets most of the cytoplasm, is
surrounded by granulosa cells and the structure is now called a secondary
follicle. The secondary oocyte starts Meiosis II producing another polar body
and a larger cell that develops into an ovum. Meiosis II is completed after
fertilization. The first polar body can also divide producing two more polar
bodies that disintegrate.
Uterine (Fallopian) tubes are the oviducts that conduct the ovum to the uterus. If fertilization occurs, it usually does so here. Their structure consists of an infundibulum, a funnel shaped opening to the ovaries and fimbriae, fringe on the infundibulum. The ampulla of the uterine is the wide portion of the tube and is about 2/3 of the length of the tube. The isthmus is the short portion that attaches to the uterus. Ciliated epithelial cells that line the inside of the tube help move the ovum to the uterus. Secretory cells nourish the ovum and create a fluid in which the ovum can move. The muscularis provides peristaltic contractions that aid in ova movement.
The uterus serves as the site of
menstruation, implantation of the fertilized ova, and development of the fetus
and labor.
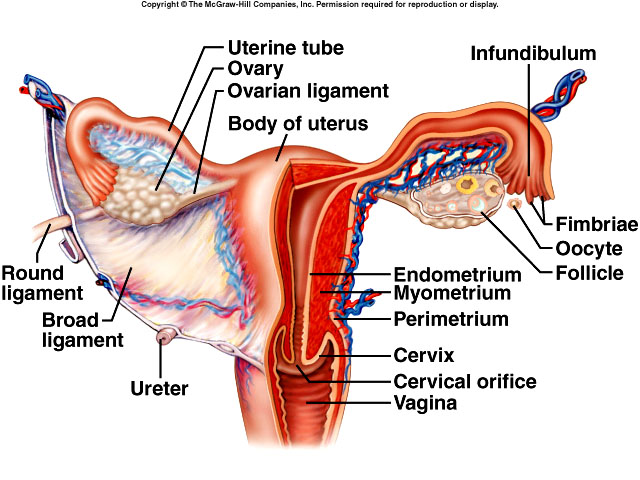 Before
the first pregnancy it is about 3” long, 2” wide, and 1” thick. The uterus
consists of the fundus, body, cervix (secretory cells produce cervical mucus
which is receptive to and protects sperm. The uterine cavity is the interior of
the body of the uterus. A cervical canal contains an internal and external
opening. The uterus is supported by the broad, uterosacral, cardinal and round
ligaments. Layers include the perimetrium, myometrium, and endometrium which can
be divided into the stratum functionalis and the stratum basalis.
Before
the first pregnancy it is about 3” long, 2” wide, and 1” thick. The uterus
consists of the fundus, body, cervix (secretory cells produce cervical mucus
which is receptive to and protects sperm. The uterine cavity is the interior of
the body of the uterus. A cervical canal contains an internal and external
opening. The uterus is supported by the broad, uterosacral, cardinal and round
ligaments. Layers include the perimetrium, myometrium, and endometrium which can
be divided into the stratum functionalis and the stratum basalis.
The vagina serves as a passageway for menstrual flow and childbirth and as a receptacle for the penis during intercourse. The fornix is the recess that surrounds the vaginal attachment to the cervix. The vaginal orifice is the opening to the vagina and may be covered by a thin membrane called the hymen. Mucosa cells contain glycogen, which when utilized cause an acid pH. Lactobacilli are the primary organisms colonizing the vagina. Vulva is a term used to describe the external female genitalia. Vulva comprise the mons pubis, major and minor labia, clitoris, vestibule, vaginal and urethral orifices, the paraurethral glands, and the greater and lesser vestibular glands. The function of the glands is to secrete fluids before and during sexual intercourse.
The perineum is a diamond shaped area between the thighs, the buttock and the genitalia of males and females. The anterior portion is called the urogenital triangle and the posterior potion, the anal triangle.
Mammary
glands are modified sweat glands located over the pectoralis major muscles.
Their function is to synthesize, secrete, and eject milk (lactation). The amount
of adipose tissue determines the size. Each contains 15-20 lobes and each lobe
consists of lobules. The alveoli glands drain the milk into secondary tubules,
then into mammary ducts to the lactiferous sinuses for storage. When ejected,
milk travels from these sinuses to lactiferous ducts and out through the nipple.
The pigmented area surrounding the nipple is called the areola. Development of
the mammary glands occurs at puberty and depends on the presence of estrogen and
progesterone. Adipose tissue is deposited, the duct system develops, and the
nipple and areola grow and become pigmented. Milk production is due the hormone
prolactin and milk ejection is due to the hormone oxytocin.
Female Reproductive Cycle
In general the reproductive cycle occurs approximately once each month in
non-pregnant females during their reproductive years. The function is to prepare
the uterus for a fertilized ovum. It involves two cycles, the ovarian cycle for
maturation of the ovum and the uterine (menstrual) cycle during which there are
changes in the endometrial lining of the uterus.
Both are controlled by hormones. Gonadatropin
releasing hormone (GnRH) from the hypothalamus stimulates the release of LH sand
FSH by the pituitary gland. FSH in turn stimulates initial development of the
ovarian follicles and secretion of estrogen. LH stimulates further development
of the follicles, ovulation, and secretion of estrogen and progesterone.
B-estradiol is the major estrogen produced. It promotes development and
maintenance of female reproductive organs, secondary sex characteristics and
development of the breasts in addition to regulating fluid and electrolyte
balance and stimulation of protein synthesis. Progesterone helps prepare the
endometrium for implantation of the fertilized ovum and prepares the mammary
glands for milk secretion. Relaxin is produced by the corpus luteum and helps
dilate the cervix to ease delivery. Inhibin is also produced by the corpus
luteum and it inhibits FSH and GnRH.
Phases of the Female Reproductive
Cycle
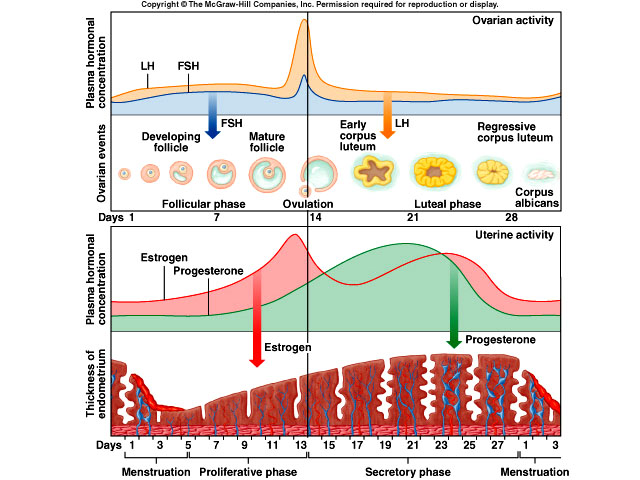 The
menstrual phase lasts @ 5 days and there is a discharge of 50-150 ml of blood,
tissue fluid, mucous, and cells from the endometrium. It is caused by decreased
levels of estrogen and progesterone which causes the blood vessels to constrict
and the stratum functionalis to slough off. The preovulatory phase occurs during
days 6 -13. This is the follicular phase during which follicles develop. In the
proliferative phase endometrial repair takes place, estrogen is secreted. Close
to the time of ovulation, an increased amount of LH is secreted (this is an
indication of imminent ovulation. Ovulation occurs about day 14 of the 28 day
cycle. The corona radiata, an oocyte which is surrounded by its zona pellucida
and covered by follicular cells is released by a secondary follicle. Other signs
of ovulation include increased basal temperature, production of clear, stretchy
cervical mucus, changes in the uterine cervix, and sometimes the presence of
ovarian pain. The postovulatory phase, days 15 - 28, is the time between
ovulation and the next menstrual cycle. During this period the endometrium
thickens awaiting the fertilized ovum. An abundant amount of estrogen and
progesterone are secreted by the corpus luteum. Progesterone causes the
endometrium to become more vascular and glandular. High levels of progesterone
and estrogen inhibit the release of FSH and LH. If fertilization does not
happen, the corpus luteum degenerates into the corpus albicans, decreasing the
amounts of estrogen and progesterone and initiating another ovarian and
menstrual cycle. About day 25, another group of primordial follicles start to
develop into primary follicles. If fertilization does occur, placental hCG
maintains the corpus luteum. Both secrete estrogen and progesterone to support
pregnancy and breast development for lactation.
The
menstrual phase lasts @ 5 days and there is a discharge of 50-150 ml of blood,
tissue fluid, mucous, and cells from the endometrium. It is caused by decreased
levels of estrogen and progesterone which causes the blood vessels to constrict
and the stratum functionalis to slough off. The preovulatory phase occurs during
days 6 -13. This is the follicular phase during which follicles develop. In the
proliferative phase endometrial repair takes place, estrogen is secreted. Close
to the time of ovulation, an increased amount of LH is secreted (this is an
indication of imminent ovulation. Ovulation occurs about day 14 of the 28 day
cycle. The corona radiata, an oocyte which is surrounded by its zona pellucida
and covered by follicular cells is released by a secondary follicle. Other signs
of ovulation include increased basal temperature, production of clear, stretchy
cervical mucus, changes in the uterine cervix, and sometimes the presence of
ovarian pain. The postovulatory phase, days 15 - 28, is the time between
ovulation and the next menstrual cycle. During this period the endometrium
thickens awaiting the fertilized ovum. An abundant amount of estrogen and
progesterone are secreted by the corpus luteum. Progesterone causes the
endometrium to become more vascular and glandular. High levels of progesterone
and estrogen inhibit the release of FSH and LH. If fertilization does not
happen, the corpus luteum degenerates into the corpus albicans, decreasing the
amounts of estrogen and progesterone and initiating another ovarian and
menstrual cycle. About day 25, another group of primordial follicles start to
develop into primary follicles. If fertilization does occur, placental hCG
maintains the corpus luteum. Both secrete estrogen and progesterone to support
pregnancy and breast development for lactation.
The physiology of sexual intercourse in the male involves erection, a
minimal amount of lubrication, and orgasm. Sexual function is controlled by the
CNS, which processes both tactile as well as psychic stimuli. Parasympathetic
impulses pass from the sacral portion of the spinal cord to the penis as a
result of sexual stimulation. These impulses dilate the arteries and constrict
veins causing the erection. When sexual stimulation peaks, sympathetic impulses
cause peristaltic contractions from the ducts in the testes to the urethra along
with stimulation of skeletal muscles at the base of the erectile tissue causing
ejaculation. In the female, sexual intercourse also involves erection, most of
the lubrication, and orgasm. Lubrication occurs from secretions into the vagina
by the paraurethral and the greater and lesser vestibular glands. Successful
orgasm is dependent on psychic and local stimulation. An orgasm may assist to
becoming pregnant. This theory based on the fact that artificial insemination is
not always successful.
Birth Control
Sterilization is the most reliable method. In the
male, a vasectomy is performed. In the female, a tubal ligation whereby the
uterine tubes are cut and the ends tied. Hormonal methods are utilized in oral
contraceptive that includes both estrogen and progesterone. An IUD is an
intrauterine device that is placed into the uterus to prevent implantation of a
fertilized ovum. Problems with the IUD have included pelvic inflammatory
disease, infertility, excess bleeding and pain. Barrier devices include the
condom, which offers some protection against STD, the diaphragm, and the
cervical cap. Chemical methods are all spermicidal agents. Behavioral methods
include the rhythm method which advocates avoiding intercourse just before,
during, and after ovulation. A symptom-thermal method is another behavioral
method in which intercourse is avoided when signs of ovulation exist. The last
behavioral method is coitus interruptus in which the penis is withdraw just
before ejaculation.
Aging and the Reproductive Systems
Puberty is a time when the secondary sex characteristics begin to develop and
the potential for sexual reproduction is reached. Male puberty starts at @ 10-11
years old and ends 15-17. Changes in testes result in maturation of
sustentacular cells and the initiation of spermatogenesis and are controlled by
an increase in FSH, LH and testosterone. Female puberty starts with the first
menses (menarche) about age 12. Increases in FSH, LH and estrogen initiate the
process.
Menopause is caused by the aging of the ovaries. It occurs between the ages of 40 - 52. It is the result of the ovaries becoming less responsive to gonadotropic hormones. Symptoms include hot flashes, hair loss, and mood swings, although 20% of women do not exhibit any symptoms. Estrogen replacement therapy may help reduce symptoms. Osteoporosis is also possible due to lower levels of estrogen.
In older men, about age 55, there is
a decrease in the levels of testosterone which causes a decrease in strength,
sexual desire, and viable sperm although men have become fathers when they are
in their nineties. Prostate disorders are common.
Sexually Transmitted Diseases (STD)
STDs are venereal diseases spread by usually by direct sexual contact. Gonorrhea
(GC) is caused by bacteria Neisseria gonorrhoeae. About 360,000 cases
were reported in 2001 in the U.S. Untreated cases can cause sterility in females
(due to scarring of the uterine tubes) and the male (scarring of the vas
deferens). Pelvic inflammatory disease can lead to peritonitis, and possibly
death, but a GC infection can also be asymptomatic which allows for transfer of
the disease. GC can cause blindness if transmitted to newborn at birth. In the
male it usually causes urethritis, with a yellow, creamy discharge and painful.
The disease is treated with antibiotics.
Syphilis is caused by bacteria Treponema pallidum. Less than 7,000 new cases were reported in 2001. Primary syphilis is manifested by a lesion on the genitalia which is a non-painful, hard chancre. Usually it heals by itself but the organism remains in the body only to emerge as secondary syphilis in which a very infectious rash covers the body. Tertiary syphilis affects organs such as the heart or the brain. Syphilis can be transmitted to the fetus (congenital syphilis) which results in a baby with many birth defects, if it survives. Syphilis can be treated with penicillin.
Chlamydia is caused by bacteria Chlamydia trachomatis. More than 780,000 cases were reported in 2001 making it the most common reportable organism in the U.S. In males it causes a urethritis; in females it can cause sterilization due to scarring of the uterine tube. This organism can also be transmitted to newborns at birth causing eye infections (blindness if untreated) and/or respiratory disease. It also can be treated with antibiotics.
Genital Herpes is caused by a virus Herpes simplex II. About a half million cases per year are reported. Genital herpes produces painful genital blisters. It can be treated with antiviral drugs but all they do is cause the organism to go into remission; one never gets rid of it.
Genital Warts are caused by the Human papilloma virus. About one million cases per year are reported. There is no cure although cryotherapy, electrocautery, laser surgery are used to remove lesions. Cervical cancer is now known to be linked to the HPV virus.
AIDS is caused by the Human Immunodeficiency Virus (HIV). HIV can be transmitted through intercourse. It is mostly found in homosexual men and drug abusers, although the greatest increase is in heterosexual females. The cumulative cases and deaths reported in the U.S. from the early 1980s through December, 2001 are 820,000 cases with 470,000 deaths. Approximately 40,000 new cases are reported each year in the U.S. There is no cure.
Trichomoniasis is caused by the parasite Trichomonas vaginalis. It causes an inflammation of the vagina or urethra and can be treated with antibiotics.
Basic treatment guidelines require treatment of both sexual partners. Condoms offer some protection but prevention through education of the disease mechanisms is better. Then there are also the behaviors of abstinence or fidelity in a monogamous relationship that prevent the spread of STDs.
PREGNANCY, GROWTH, & DEVELOPMENT
Development during Pregnancy
For fertilization to occur, a sperm must
penetrate an ovum within 24 hours of ovulation. Sperm invade the
follicular cells and bind to the zona pellucida. Fertilization of the
ovum by a sperm cell results in the formation of a zygote. Once this happens
additional sperm are prevented from penetrating the oocyte. Completion of female
meiosis occurs only after the sperm enters the egg. Even under optimum
conditions, pregnancy only occurs about 25% of the time. Research indicates that
about 50% of the fertilized zygotes are lost. Of the successful pregnancies, 20%
will result in a
miscarriage. Most of the miscarriages are due to
chromosomal abnormalities in the zygote.
The period of cleavage is the first
period in the prenatal period. Cleavage is defined as cellular divisions.
Dizygotic (fraternal) twins are the result of independent release of two oocytes
whereas monozygotic (identical) develop from a single fertilized ovum. The formation
of the morula occurs about 3 days after fertilization, multiple cellular
divisions and the arrival at the uterus. The zona pellucida disintegrates.
Development of the blastocyst, a hollow ball of
cells that implants in the endometrium occurs about six days after
fertilization, begins. The blastocyst has an outer covering called a trophoblast
that eventually develops into the chorion. The inner cell mass develops into the
embryo proper.
Hormones of Pregnancy
Hormones that maintain pregnancy are hCG (Human chorionic gonadotropin) that
helps prevent spontaneous abortion by maintaining the corpus luteum which
continues to secrete estrogen and progesterone which in turn prevents the
release of FSH and LH. Placental lactogen stimulates breast development. Relaxin
relaxes joints and ligaments to facilitate easier delivery. hCG is the hormone
detected in pregnancy tests.
Embryonic development occurs from the second week through the eighth week of development. The beginning of the organ systems occur during embryonic development. The primary germ layers are, initially the ectoderm and endoderm layers (form embryonic disc), and eventually the mesoderm which develops in between. The endoderm becomes endothelial lining of GI tract and other accessory organs. The mesoderm forms muscles, bone and other connective tissue and the peritoneum. The ectoderm develops into the skin and nervous tissue.
Embryonic
membranes
The yolk sac is the primary source of nourishment to developing embryo and early
source of blood development as a result of the embryo receiving nutrients from
endometrium of uterus. The amnion becomes amniotic sac and is filled with
amniotic fluid. The chorion becomes the embryonic part of the placenta. The
allantois develops into to the blood vessels of the umbilical cord. The placenta
and umbilical cord are expelled after birth.
The fetal stage begins at the eighth week and terminates at
birth. Certain periods during the fetal stage, the fetus is very susceptible to
specific
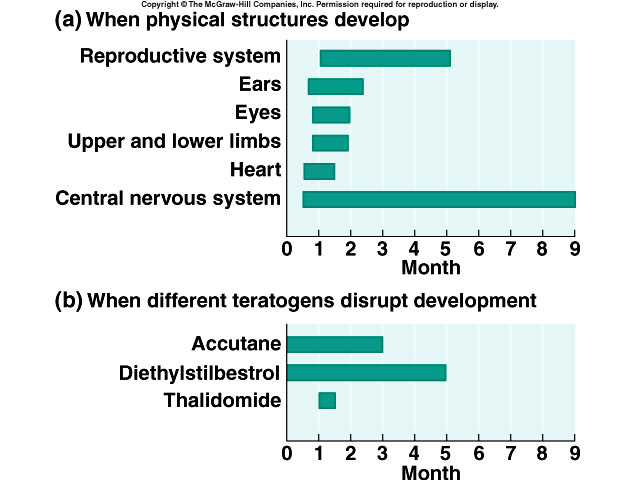 teratogens
which affect certain organs of development. The first two months are very
important to organ development. However, during the entire fetal stage, the
fetus’s central nervous system is susceptible to developmental disruption.
teratogens
which affect certain organs of development. The first two months are very
important to organ development. However, during the entire fetal stage, the
fetus’s central nervous system is susceptible to developmental disruption.
During gestation the fetus grows and develops. The circulatory system in the fetus is slightly different than the one after birth. Prior to birth the maternal blood supply provides nutrients and oxygen and carries away wastes which diffuse thought the placenta. One half of the blood traveling into the fetus via the umbilical vein goes to the fetal liver while the other half goes via the ductus venosa to the inferior vena cava. From the heart most of the blood goes from the pulmonary trunk via the ductus arteriosus to the aorta to go to the rest of the body. The blood then returns via the iliac arteries to the placenta in umbilical arteries. The small amount of blood that does go to the lungs, returns to the heart and leaves the heart via the aorta. At birth the foramen ovale between the atria of the fetal heart closes by the closing of two flaps of tissue that fuse and becomes the fossa ovalis. The ductus arteriosus closes almost immediately and usually within three months after birth becoming the ligamentum arteriosum. The ductus venosa closes becoming the ligamentum venosum. The respiratory system in the fetus depends on mom but at birth it immediately takes over by itself.
Birthing
Process
Dilation normally lasts 6-12 hours. Regular contractions of the uterus prepare
the uterus for birth. The amniotic sac ruptures. Birth can last 10 minutes to
several hours, and is characterized by complete cervical dilation. The placental
stage lasts anywhere from 5-30 minutes after delivery. The placenta is expelled
due to powerful uterine contractions.
GENETICS AND GENOMICS
DNA Code
The total amount of DNA in a cell is its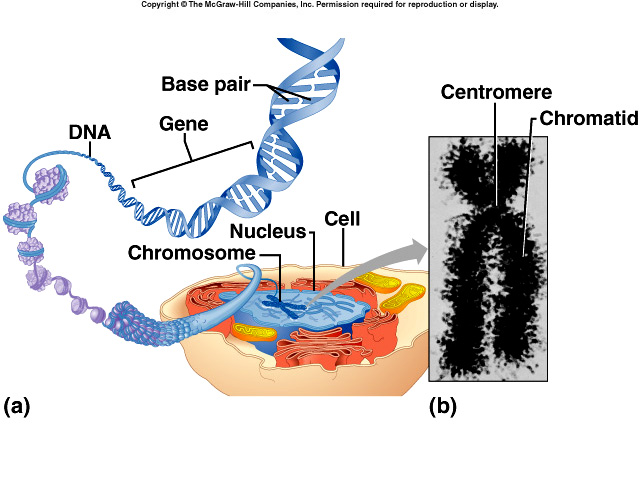 genome. DNA is the blueprint that tells the cell through RNA what proteins to
make. DNA is composed of two strands of nucleotides. The nitrogenous bases are
the purines (adenine & guanine) and pyrimidines (cytosine & thymine). They pair
up as A-T or C-G only. Deoxyribose is the sugar present. DNA forms a double
alpha helix (a twisted ladder formation). Sections of DNA are the genes (a
certain segment of DNA that contains the necessary code to make a protein or RNA
molecule). DNA maintains the genetic code during reproduction and still provides
variability. A protein’s primary structure, the order and type of amino acids in
the chain, determines its shape and function. Phenotype is the expression of a
gene.
genome. DNA is the blueprint that tells the cell through RNA what proteins to
make. DNA is composed of two strands of nucleotides. The nitrogenous bases are
the purines (adenine & guanine) and pyrimidines (cytosine & thymine). They pair
up as A-T or C-G only. Deoxyribose is the sugar present. DNA forms a double
alpha helix (a twisted ladder formation). Sections of DNA are the genes (a
certain segment of DNA that contains the necessary code to make a protein or RNA
molecule). DNA maintains the genetic code during reproduction and still provides
variability. A protein’s primary structure, the order and type of amino acids in
the chain, determines its shape and function. Phenotype is the expression of a
gene.
RNA Code
RNA is composed of single strands of nucleotides. The nitrogenous bases of RNA
are the purines (adenine & guanine) and pyrimidines (cytosine and uracil). The
sugar is always ribose. There are a number of types of RNA, each with a
different function. Messenger RNA (mRNA) is produced from DNA patterns in
transcription. The master DNA code is first copied onto mRNA through
transcription. Transfer RNA (tRNA) converts the master code on mRNA into a
specific amino acid. There are 64 varieties of codons determined by anti-codons
(nucleotide triplets) and amino acid binding sites. 61/64 represent some type of
amino acid; the other types are start or stop codons. Ribosomal RNA (rRNA) forms
the major part of the ribosome and participates in protein synthesis.
Transcription produces mRNA using the DNA code by complimentary base pairing and
occurs within the nucleus. mRNA attaches to ribosome. tRNA anticodons attach to
complimentary codons of mRNA amino acids join to produce protein. Translation is
the production of a protein from a mRNA strand. All elements needed to
synthesize a protein are brought together on the ribosome. Translation occurs in
the cytoplasm.
Mutation Mechanisms
A mutation is a permanent change in the DNA that may be passed along from
generation to generation. The wild type gene exhibits normal characteristics. A
mutant gene usually causes disease or an unusual trait to be expressed. Causes
of mutation can be spontaneous, a random change in DNA that arises from mistakes
in DNA replication or induced due to chemical or physical factors. Induced
mutations usually result in cell death but can lead to cancer.
Categories of mutations include point
mutations (a change the nature of one gene, called a frameshift mutation is
brought about by the deletion or insertion of a base pair), a substitution
mutation (a wrong base pair is put in place of correct bp producing error in
base pairing, thus a change in the codon), an inversion mutation (change in one
or two codons whereby adjacent base pairs change position). Mutations can be
silent (no change in amino acid), missense with consequences from none to
severe, or nonsense which leads to a STOP codon. Large mutations are ones in
which whole chromosomes are lost or large genetic sequences are inserted and are
usually fatal. What genetic mutations in higher animals, such as humans, done to
enhance the species? (For example, the ability to form speech and larger brains
leading to civilization?)
Emerging Role of Genetics
Genetics is the study of trait transmission through DNA passed by the
gametocytes from generation to generation. Factors that influence development of
individual characteristics are heredity and environment. Environment can cause
the expression of genes. Genes are part of chromosomes. They encode proteins.
DNA makes RNA makes proteins. Genomics considers heredity in terms of genes that
interact with one another and the environment. Proteinomics considers how
proteins interact within the body.
Modes of Inheritance
A genome is the entire DNA in the cell of an organism. Genotype is the
combination of genes within a cell or organism. Phenotype is the physical
expression of the genotype. Humans have 22 pairs of autosomes and one pair of
sex chromosomes (XY). An allele is different forms of a gene found at the
same locus (pl. loci) of a paired chromosome. Homologous chromosomes are
identical.
Dominant and Recessive Inheritance
If a gene is dominant, that characteristic is expressed even when heterozygous
genes are present. Dominant genes determine the phenotype. If a gene is
recessive, the only way this characteristic can be expressed is if it is
homozygous. Otherwise the trait is usually masked. Heterozygous means having a
dominant and a recessive gene. Sometimes genes are co-dominant that is, two
genes, and share dominance such as in AB blood type. Incomplete dominance occurs
when the heterozygous phenotype is intermediate between that of either gene.
Neither is dominant over the other.
Matters of Sex
Sex is determined at conception by the male gamete. Traits transmitted on X
chromosome are X-linked those on the Y-chromosome are Y-linked. Y-linked traits
are only transmitted from fathers to sons. Gender effects on phenotype.
Sex-limited trait affects a structure or a function that is present only in
females or in males. Sex-influenced inheritance the allele is dominant in one
sex but recessive in the other. Difference in expression is due to hormones.
Genomic imprinting is the expression of the disorder is dependent on which
parent transmits the disease causing gene.
Disorder terms
Completely penetrant indicates that everyone who has the gene will express it,
whereas is a person exhibits incomplete penetrance; they will only have some
symptoms. Variably expressive means symptoms vary in intensity in different
people (severity). Pleiotrophy occurs when a single genetic disorder can produce
several symptoms. (Marfan syndrome affects elastic connective tissue). Complex
traits indicate that one or more genes plus the environment mold multifactorial
traits. Examples include height and skin color, heart disease, and cancer.
Chromosome Disorders
Polyploidy means that greater than two sets of chromosomes are produced. This is
incompatible with life if in embryo.
Aneuploidy refers to cells missing a chromosome
or having an extra one. This results from nondisjuncture in meiosis. Monosomy in
humans is 45 chromosomes (Turner’s syndrome XO). Trisomy in humans is 47
chromosomes. Examples include Down’s syndrome (Trisomy 21), Trisomy 18, Trisomy
13, and Klinefelter’s syndrome XXY.
Prenatal
tests to check for possible genetic problems are amniocentesis, chorionic
villus sampling, and fetal cell sorting. All carry somewhat of a risk to the
fetus.
Gene Therapy can be
heritable gene therapy or non-heritable gene therapy.





