
CARDIOVASCULAR SYSTEM: THE BLOOD
FUNCTION OF BLOOD
Blood transports gases and nutrients throughout the body and transports wastes
to the lungs, kidneys and skin for elimination from the body. Circulating blood
helps maintain homeostasis in all body fluids. Blood regulates pH via acid-base
buffering system. Blood protects against blood loss by its ability to form
clots. Lastly many blood components protect the body against disease.
Blood is divided into two components: plasma and formed elements.
Plasma contains water, proteins (albumin, globulin, and fibrinogen),
electrolytes, nutrients, gases, enzymes, wastes. The
formed elements include
erythrocytes (red blood cells), leukocytes (white blood cells) and thrombocytes
or platelets.
The process of forming blood cells is called hemopoiesis. Hematopoietic growth factors (Erythropoietin, colony stimulating factors, and Thrombopoietin) stimulate proliferation of various cell types. A hemocytoblast (hemopoietic stem cell) differentiates into other cell types in the bone marrow. Rubriblasts form erythrocytes. Monoblasts form monocytes. Lymphoblasts form lymphocytes. Megakaryocytes form platelets.
Erythrocytes are biconcave disc whose function is to carry oxygen to the cells and tissues of the body. Their life span is about 120 days and number produced each day equals the number destroyed. Normal hemoglobulin levels are: (infant 14-20 g/100 ml of blood), female (12-16), male (13.5-18), Hematocrit (3x hemoglobin). Red cell counts are important values the physician looks at in maintaining homeostasis in the patient.
Events in hormonal control
When the kidney and liver experience oxygen deficiency they release
erythropoietin. Erythropoietin travels to bone marrow and stimulates increased
production of RBC. As more RBC are released into bloodstream, O2
carrying capacity increases taking more O2 to the liver & kidneys
causing a decrease in release of erythropoietin.
Dietary factors affecting RBC
production include vitamin B12 and folic acid affect DNA synthesis.
Iron affects hemoglobin synthesis.
The white blood cells are also known as Leukocytes. There are two types: granulocytes (granules in cytoplasm) and agranulocytes (no granules in cytoplasm). Granulocytes can be further subdivided into neutrophils (PMN whose function is to phagocytize bacteria and fungi), eosinophils (associated with allergic reaction and parasitic worm infestations), and basophils (release histamine that promotes inflammation). There are two types of agranulocytes: Monocytes (phagocytize bacteria, dead tissue) and Lymphocytes (form antibodies, destroy foreign material directly). WBC life span varies from less than one day to years depending on cell type. A differential count provides the percentages of WBC in the blood. A normal differential will contain 54-62% PMN, 1-3% Eosinophils, <1% Basophils , 25-33% Lymphocytes, and 3-9% Monocytes.
Leukocytosis refers to a WBC count of >10,000/mm whereas leucopenia is defined as a WBC count of <5,000/mm.
Thrombocytes or platelets function in control of blood loss (130-360,000).
Hemostasis
Hemostasis refers to the stoppage of bleeding. The steps of
hemostasis are:
-
Vascular spasm whereby the ends of blood vessels contract by themselves to stop bleeding.
-
Platelet plug formation in which the platelets adhere or stick to ends of injured blood vessels and to each other.
-
Coagulation follows two pathways (extrinsic and intrinsic) that end up in the same place with the formation of prothrombinase. From this point a common pathway (stage 2 is the conversion of prothrombin into thrombin) is followed. Stage 3 is the conversion of soluble fibrinogen into insoluble fibrin.
-
Finally there is Clot retraction.
Haemostatic control mechanisms are regulated by both positive and negative feedback mechanisms. As the clot is being formed, each step activates the formation of a new factor. Once the damage has been repaired a negative feedback system is activated to destroy and remove the clot (fibrinolytic system). This negative feedback also prevents intravascular clotting.
Blood grouping (typing)
Blood groups are
determined by the presence or
absence of antibodies on the cell membrane. There are
four groups A, B, AB and O
which are determined by the expression of genes a person inherits. A person with Type AB is
considered the universal recipient because cells lack antibodies to types A & B
blood. People with Type O blood are called the universal donors because their
blood lacks antigens for type A, B, and AB. Another group that was named after
the rhesus monkey is the
Rh group. If an Rh-negative woman and an RH-positive man
conceive a child, there is the possibility of developing a child with a disease
called Erythroblastosis fetalis or hemolytic disease of the newborn (HDN) in
subsequent conceptions. Note: this does not affect the first conception.
THE CARDIOVASCULAR SYSTEM: THE HEART
Anatomy of the Heart
The heart rests on the diaphragm in a space called the mediastinum. It weighs @
300 grams and is about as big as a clenched fist. The pointed end is called the
apex and the opposite end is called the base but is really the top of the heart.
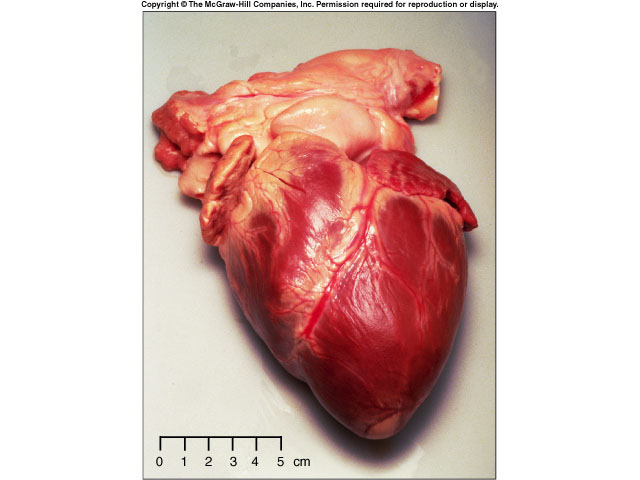 The bulk of the heart is made up of the left ventricle. A pericardium (a
3-layered bag) surrounds the heart and composed of fibrous pericardium (that
provides protection to the heart, prevents overstretching, and anchors the heart
in the mediastinum), a serous pericardium which is composed of two layers (the
parietal layer or outer layer that is fused to the fibrous pericardium and the
visceral layer or the inner layer that adheres to heart muscle) The visceral
pericardium is also called the epicardium. Pericardial fluid is found in
the pericardial cavity which is located between the two layers and helps
lubricate and reduces friction between membranes as the heart moves.
The bulk of the heart is made up of the left ventricle. A pericardium (a
3-layered bag) surrounds the heart and composed of fibrous pericardium (that
provides protection to the heart, prevents overstretching, and anchors the heart
in the mediastinum), a serous pericardium which is composed of two layers (the
parietal layer or outer layer that is fused to the fibrous pericardium and the
visceral layer or the inner layer that adheres to heart muscle) The visceral
pericardium is also called the epicardium. Pericardial fluid is found in
the pericardial cavity which is located between the two layers and helps
lubricate and reduces friction between membranes as the heart moves.
The heart wall is composed of three layers: the epicardium (see visceral pericardium above), the myocardium which is cardiac muscle tissue and the bulk of mass in the heart and endocardium or the innermost layer of the heart. This lining is continuous through all of the blood vessels except for the capillaries.
The Heart Chambers and Valves
Internally the heart is divided into four chambers the two
upper chambers are the right and left atria. Each has an appendage (auricle)
whose function is to increase the volume of the atria. Atria have thin walls
because they deliver blood only to the ventricles. The two lower chambers are
called the right and left ventricles. The left ventricle is two to four times as
thick as the right ventricle because it has to pump blood to the entire body
whereas the right ventricle pumps blood only to the lungs. An interventricular
septum separates the ventricles and an interatrial septum separates the atria.
The interatria septum also contains the Fossa ovalis which is the site of
the foramen ovale, an opening in the fetal heart. Trabeculae carneae are
folds and ridges of the myocardium in the ventricles.
The heart valves function to prevent the backflow of blood. They open and close in response to pressure changes. These atrioventricular valves lie between the atria and the ventricles. The Tricuspid valve is on the right side and the Bicuspid valve (mitral valve) is on the left side. Chordae tendineae connect the valves to the papillary muscles. Blood moves from the atria to the ventricles when pressure is low in the ventricles. When the ventricles contract, the AV valves are forced closed and the chordae tendineae prevent the valve from eversion into the atria. The pulmonary semilunar valve lies in the opening where the pulmonary trunk leaves the right ventricle and the aortic semilunar valve lies at the opening of the left ventricle and the aorta. Because there are no valves between the atria and the veins some of the arterial blood is forced back into the veins.
Blood Flow Through the Heart
Deoxygenated blood comes from the superior and inferior
vena cava and the coronary sinus into the right atrium which then pumps blood into
the right ventricle. From the right ventricle, blood is pumped to the lungs via
the left and right pulmonary arteries. Blood returns from the lungs via the two
left and two right pulmonary veins to the left atrium which then pumps the blood
into the left ventricle. From the left ventricle, blood is pumped to the
systemic circulation via the aorta. The Ligamentum arteriosum is
a remnant
of a fetal blood vessel that passed blood from the pulmonary trunk to the arch
of aorta bypassing the lungs.
Heart Blood Supply
Coronary arteries transport blood to the heart. The left
coronary artery branches into the anterior interventricular branch which
supplies both ventricles and the circumflex branch which supplies left atrium
and left ventricle. The right coronary artery supplies the right atria with
small branches, then branches into the marginal branch which supplies the right
ventricle and the posterior interventricular branch that supplies both
ventricles. The coronary veins, specifically the great cardiac vein and the middle
cardiac vein drain blood into the coronary sinus which empties into the right
atrium. The blood vessels lie in a coronary sulcus which is an external groove
that separates the atria from the ventricles and in the anterior and posterior interventricular sulcus which are external grooves that separate the ventricles.
Cardiac Cycle
The cardiac cycle describes pressure, volume and flow phenomena in the
atria and ventricles over time. Phases of the cardiac cycle consist of systole
(contraction) and diastole (relaxation) of both atria and both ventricles. When
atria contract, the ventricles are relaxed and when the ventricles contract, the
atria are relaxed. During the relaxation period at the end of a heartbeat
blood flows from the pulmonary trunk and the aorta back toward the ventricles,
so the semilunar vales close causing a dicrotic wave on the aortic pressure
curve. This is represented by the T-wave on the ECG, atria and ventricles are
relaxed, pressure drops in the ventricles. When both the semilunar valves and
the AV valves are closed, no blood enters the ventricles. This is known as
isovolumetric ventricular relaxation.
Ventricular filling occurs when the ventricular pressure falls below atrial pressure and the AV valves open rapid filling the ventricles. During diastasis a small amount of blood enters the ventricle. During atrial systole about 30 cc of blood is added to the ventricle. During ventricle systole, ventricular ejection occurs when the left ventricle pressure surpasses aortic pressure (@ 80 mm hg) and right ventricular pressure exceeds pressure in the pulmonary trunk (@ 15-20 mm hg). Just prior to ventricular contraction is the isovolumetric contraction. All valves are closed again. Atrial filling occurs continuously during the cardiac cycle except during atrial systole.
Heart Sounds (auscultation)
During each cardiac cycle four sounds are generated but you
can only hear the first two. Lubb, the first sound is the loudest and is created
by blood turbulence associated with closing of the AV valves. Dupp, the
second sound, is associated with closing of semilunar valves. Heart murmur
is an
abnormal sound that consists of a flow noise that is heard before, between, or
after lubb-dupp sounds or it may mask the normal heart sounds. Often it
indicates a valve disorder such as mitral stenosis, mitral insufficiency, aortic
insufficiency, or mitral valve prolapse.
Conduction system and Pacemaker
For the heart to act as an efficient pump for blood
circulation it's important that there is a precise and sequential activation of
contraction of the atria and the ventricles during each heart beat. Autorhythmic
cells are self excitable cardiac muscle fibers that act as a pacemaker for the
entire heart and form the conduction system or the route for conducting impulses
throughout the heart. The components are the Sinoatrial node (SA) located in the
upper right atrial wall, the Atrioventricular node in lower interatrial septum,
the Atrioventricular bundle (bundle of his) which electrically connects atria
and ventricles, the right and left bundle branches that are located in
interventricular septum and conduction myofibers (purkinje fibers) that conduct
impulses into ventricular muscle mass. Electrical impulses from the SA node pass
through the atria stimulating atrial contraction. The impulse is delayed at the
AV node and then passes through the rest of the conduction system causing
ventricular contraction when it enters the ventricular muscle mass. The impulse
doesn't go straight through the entire heart because of a layer of connective
tissue that insulates the atria from the ventricles. The delay at the AV node is
important because it allows the ventricles to fill with blood. If the SA node is
damaged, the AV node and rest of system will compensate somewhat but not
enough. The person needs a pacemaker implant.
Electrocardiogram (ECG or EKG)
An ECG is a record of electrical changes during each
cardiac cycle. It does not measure mechanical performance of the heart. It is
used to determine if the conduction pathway is normal, if the heart is enlarged,
and if certain regions are damaged. A normal ECG consists of a P-wave (atrial
depolarization) when the atria contract, a QRS-complex (ventricular
depolarization) when the ventricles contract, and a T-wave (ventricular
repolarization) when the ventricles relax.
BLOOD VESSELS AND HEMODYNAMICS
Arteries carry blood from the heart to the tissues. They branch into medium size arteries that in turn branch into arterioles. Arterioles branch into capillaries in which substances are exchanged with the tissues through the walls of the capillaries. The capillaries unite to form venules, which in turn unite to form veins. Veins transport blood back to the heart. Vasa vasorum are the blood vessels that carry oxygen and nutrients to the vessels.
Anatomy of Blood Vessels
Arteries have three layers. The tunica interna is the inner
wall. The tunica media (middle layer) is composed of elastic fibers and smooth
muscle. The tunica externa is the outer wall and is composed of elastic and
collagen fibers. A lumen is the hollow center of the vessel for blood flow. The functional
properties of arteries are elasticity that allows blood vessels expand to
accommodate the blood expelled during ventricular contraction and contractility;
vasodilation is an increase in vessel size whereas vasoconstriction is a
decrease in vessel size.
Arterioles are very small microscopic arteries that deliver and regulate blood to the capillaries through vasoconstriction (smooth muscle of arteriole contracts) and vasodilation (smooth muscle of arteriole relaxes). They are also composed of same three tissue layers as the arteries.
Capillaries connect the arterioles to the venules and are found near almost every cell in the body. Their function is to permit the exchange of nutrients, gases and wastes between blood and tissue cells. The cell walls have only one layer, an endothelial cell. A metarteriole is a vessel that originates at an arteriole and empties into a venule and functions in bypassing capillary beds when those capillaries are not used; therefore serve as a low resistance path for blood flow. True capillaries emerge from an arteriole or metarteriole but are not on the direct path of arteriole to vein. Precapillary sphincters control the flow of blood into the capillary.
The most important mechanism for exchange of nutrients and wastes in the capillaries is diffusion from a higher concentration to lower. Other methods include vesicular transport (transcytosis) whereby substances become enclosed in tiny vesicles that enter the endothelial cells by endocytosis and leave by exocytosis. Another method is bulk flow (filtration and reabsorption). This is a passive process that involves the movement of large number of ions, molecules or particles in the same direction. Normally filtration from one end of the capillary will equal reabsorption at the other end (Starling's Law of the capillaries). Sometimes edema occurs when the rate of fluid filtration out of the capillary bed exceeds the ability of the lymphatic drainage system to return filtered fluid to the vascular system.
Veins and Venules
Capillaries combine to form small veins called venules.
Venules unite to form veins. They are composed of the same three layers as
arteries except that the tunica interna and tunica media are thinner and the
tunica externa is thicker than those found in arteries. Veins in the limbs
contain valves that prevent the backflow of blood. Veins and venules
serve as the main blood reservoirs because they hold @ 60% of the blood in the
body.
Hemodynamics: Physiology of Circulation
The volume of blood that flows through any tissue in any
given time period is called blood flow. The velocity decreases as it flows from
the arteries to arterioles to capillaries (increasing resistance) and increases
as it leaves capillaries on return trip to the heart through venous system
(decreasing resistance). The time it takes for the blood to complete the entire circuit
is @ 1 minute. The volume of blood flow or cardiac output is equal to 5.25 l/min.
Factors that influence output include blood pressure which is the pressure
exerted on a blood vessel wall by blood and resistance which is the opposition
to blood flow as a result of friction between blood and blood vessels. Blood pressure
(BP) equals cardiac output times peripheral resistance. In the aorta BP is
usually 120/80 (systolic/diastolic). Resistance to blood flow is highest in the
arterioles causing BP to decrease from 85 mm Hg to 35 mm Hg. By the time blood
reaches the right atrium, BP = 0 mm Hg.
Factors that influence resistance are blood viscosity, total blood vessel length, and blood vessel radius. The major function of the arterioles is to control systemic vascular resistance by dilation or constriction.
Venous return refers to the amount of blood flowing back to the heart. At steady state, venous return and cardiac output must be equal. Blood flows toward the atria because pressure at atria is 0 mm Hg. Other mechanisms that help venous return include the skeletal muscle pump whereby contraction of leg muscles drives blood toward heart and the respiratory pump in which the movement of the diaphragm causes pressure changes in the thoracic cavity which drives blood toward heart
Control of blood pressure and blood flow is done through negative feedback systems that control BP by adjusting heart rate, stroke volume, systemic vascular resistance, and blood volume. Blood flow to the brain remains constant. The Cardiovascular Center, found in the medulla of the brain, receives inputs from higher brain regions, baroreceptors (pressure sensitive sensory neurons), and chemoreceptors (monitor CO2, O2 and pH). It sends outputs to both sympathetic and parasympathetic fibers of the autonomic nervous system. Sympathetic stimulation increases heart rate and contractility. Parasympathetic impulses decrease heart rate. Autoregulation refers to local automatic adjustment of blood flow to any given region is driven mainly by the tissue's need for oxygen.
Shock and Homeostasis
Shock is an inadequate cardiac output that results in a
failure of the CVS to deliver enough nutrients and O2 to body cells. Signs
include cool, clammy pale skin due to vasoconstriction, tachycardia, weak but
rapid pulse, sweating, hypotension, and altered mental status due to cerebral
ischemia. The stages of hypovolemic shock due to blood or plasma loss. In Stage I
(compensated), symptoms are minimal and can be reversed even with as much as a
10% blood loss. Stage II (decompensated and progressive) occurs when blood volume
drops >15-25%. Compensatory mechanisms cannot maintain adequate perfusion and
the person needs medical help else positive feedback systems will contribute to
decreasing cardiac output. Stage III is irreversible. Stage III Shock leads to
certain death.
Circulatory Routes
In the Pulmonary Circuit, the lungs receive blood
from the heart via the pulmonary arteries and send it back to the heart via
pulmonary veins. The main difference between pulmonary circulation and systemic
circulation is that pulmonary arteries carry deoxygenated blood and pulmonary
veins carry oxygenated blood whereas systemic arteries carry oxygenated blood
and systemic veins carry deoxygenated blood. The Systemic circulation carries
blood from the left ventricle throughout the body and returns blood to the right
atrium.
Arteries
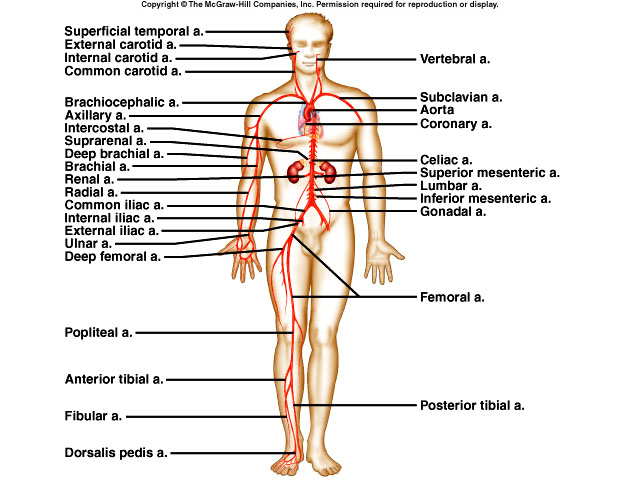 Blood vessels are continuous with branches coming off of
arteries and arterioles. The names of the vessels change based on their location
in the body. Arteries get smaller as they carry blood away from the heart. The
first portion of the aorta is the ascending aorta. From it branches the L/R
coronary arteries that supply blood to the heart. The ascending aorta becomes the
aortic arch. The brachiocephalic trunk which branches into the right common
carotid (that gives rise to the internal and external carotid artery), the right
subclavian artery, and the left common carotid artery (gives rise to the
internal and external carotid artery) all come off the arch.. Inside of the
brain the L/R internal carotids along with the basilar artery form the
circle of
Willis. Associated with the circle of Willis are the posterior and anterior
communicating arteries. The function of the circle of Willis is to equalize BP
to the brain and produce alternate routes of blood flow to the brain. As the
aorta descends it becomes the thoracic aorta above the diaphragm and then
the abdominal aorta below the diaphragm. The thoracic aorta supplies the
pericardial, esophageal, bronchial and mediastinal viscerally and the
intercostal, costal, superior phrenic branches parietally.
Blood vessels are continuous with branches coming off of
arteries and arterioles. The names of the vessels change based on their location
in the body. Arteries get smaller as they carry blood away from the heart. The
first portion of the aorta is the ascending aorta. From it branches the L/R
coronary arteries that supply blood to the heart. The ascending aorta becomes the
aortic arch. The brachiocephalic trunk which branches into the right common
carotid (that gives rise to the internal and external carotid artery), the right
subclavian artery, and the left common carotid artery (gives rise to the
internal and external carotid artery) all come off the arch.. Inside of the
brain the L/R internal carotids along with the basilar artery form the
circle of
Willis. Associated with the circle of Willis are the posterior and anterior
communicating arteries. The function of the circle of Willis is to equalize BP
to the brain and produce alternate routes of blood flow to the brain. As the
aorta descends it becomes the thoracic aorta above the diaphragm and then
the abdominal aorta below the diaphragm. The thoracic aorta supplies the
pericardial, esophageal, bronchial and mediastinal viscerally and the
intercostal, costal, superior phrenic branches parietally.
Branches off the abdominal aorta include the celiac (gives rise to the gastric, splenic, and hepatic arteries), phrenic, superior and inferior mesenteric, suprarenal, renal, and gonadal arteries.
In the arm, the subclavian artery becomes the brachial artery then divides into the radial and ulnar arteries.
Arteries of the Pelvis and Lower Extremities
The abdominal aorta divides to become the common iliac
which divides to become the internal iliac and external iliac which becomes the
femoral and then the popliteal. The popliteal divides into the anterior and
posterior tibial.
Veins
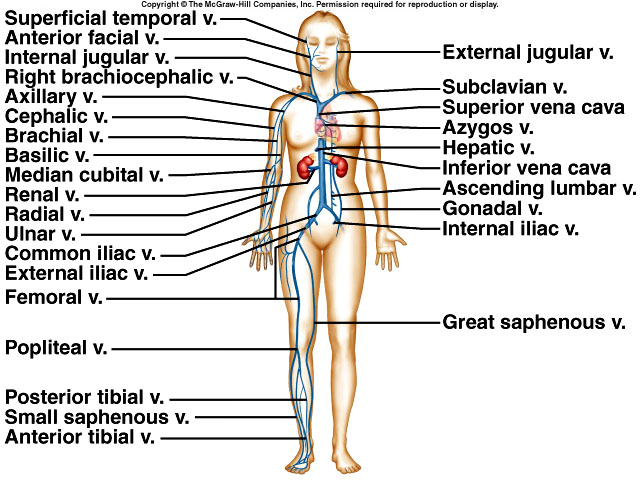 Veins bring blood to the heart. Venules merge to become larger
veins. Most (60%) of the blood in the body is stored in the venous system. The
main veins that empty into the heart are the coronary sinus that drains heart
blood, the superior vena cava which drains blood from upper regions and the
inferior vena cava that drains blood from lower regions.
Veins bring blood to the heart. Venules merge to become larger
veins. Most (60%) of the blood in the body is stored in the venous system. The
main veins that empty into the heart are the coronary sinus that drains heart
blood, the superior vena cava which drains blood from upper regions and the
inferior vena cava that drains blood from lower regions.
Veins of the Head and Neck
The exterior jugular drains blood from superficial
structures and from deep face veins into the subclavian veins as does the
vertebral vein. The internal jugular drains blood from the brain. The subclavian
joins the internal jugular to form the brachiocephalic. The R/L brachiocephalic
unite to form the superior vena cava which empties into the right atrium of the
heart.
Veins of the upper Extremities
The dorsal venous arch (DVA) drains into the basilic which
drains into the axillary and into the cephalic which merges with the accessory
cephalic to form the upper cephalic vein and that drains into the axillary. The
palmer venous arch drains into the median antebrachial which drains into the
median cubital (used in phlebotomy, IV) which unites with the basilic and drains
into the axillary at about the first rib. In the deep veins of the
upper extremities, the dorsal metacarpal drains into the radial which drains
into the brachial as does the ulnar which drains into the brachial. As mentioned
before, the brachial drains into the axillary which drains into the subclavian.
Veins of the Thorax
The zygous system drains blood from the thoracic veins and
can serve as an alternate pathway to the inferior vena cava. The azygous begins
as a continuation of the right ascending lumbar vein and receives blood from the
left intercostal, esophageal, mediastinal, pericardial and bronchial veins and
empties into the superior vena cava. The hemiazygous receives blood
from some of the intercostal veins, some esophageal and mediastinal veins and
empties into the azygous. The accessory hemizygous receives blood from the
upper left intercostal veins and the left bronchial and empties into the azygous.
Veins of the Abdomen and Pelvis
The lumbar, hepatic, suprarenal, right gonadal and renal
veins all drain into the inferior vena cava. The left gonadal drains into the
left renal.
Veins of the Lower Extremities
The deeper veins of the legs (anterior and posterior tibial) unite to
form the popliteal. The small saphenous vein empties into the popliteal vein
which then joins the femoral vein. The great saphenous (longest vein in the
body) also joins the femoral vein. The femoral becomes the external iliac. The
internal iliac unites with the external iliac to form the common iliac. The R/L
common iliac veins unite to form the inferior vena cava.
Hepatic Portal Circulation
In addition to receiving
arterial blood via the hepatic artery, much venous blood is drained through the
liver. Blood from the gastrointestinal tract and the spleen is sent to the liver
where the liver stores nutrients from digested and absorbed food, detoxifies
harmful substances, and destroys bacteria by phagocytosis. Blood from the right gastric, pyloric,
right gastroepiploic, vessels from the small intestine and the right side of the
large intestine drain into the superior mesenteric vein. Vessels from the left
side of the large intestine drain into the inferior mesenteric which joins the
splenic vein. Also adding tributaries to the splenic are vessels from the left
of the stomach. The splenic and the superior mesenteric unite to form the
hepatic portal vein. The cystic vein (from the gallbladder) also flows into the
hepatic portal vein. All blood drains from the liver via the hepatic vein into
the inferior vena cava.
THE LYMPHATIC SYSTEM
The Lymphatic System is comprised of lymph (same as interstitial fluid but is found in lymphatic vessels), thymus gland, spleen, and bone marrow (site of lymphocytic production). The function of the lymphatic system is to drain interstitial fluid, transports dietary fats which are absorbed by the GI tract, and to protect against microbe infection - the immune response. T-cells (lymphs) release cytotoxic substances that kill invaders and B-cells differentiate into plasma cells that make antibodies.
Lymphatic
capillaries and vessels
Lymphatic
capillaries begin as closed-ended vessels in interstitial spaces and are found
throughout the body. The capillaries unite to form larger lymph vessels and can
usually be found near veins in subcutaneous tissue and near arteries in the
viscera. The interstitial fluid flows into lymph capillaries but not out because
the vessels are structurally adapted to ensure the return of proteins to the
venous system. Anchoring filaments attach endothelial cells to surrounding
tissue. Backflow is prevented by valves in lymph capillaries and lymph is forced
to return towards the subclavian veins by milking action of skeletal muscles. Lymph vessels unite to form
trunks
(larger lymph vessels). The major trunks are the lumbar, intestinal, subclavian,
bronchomediastinal, and jugular which drain lymph from lymph capillaries and
pass it into two main channels. The Thoracic duct (Left
lymphatic duct) is the main collecting duct in the body. It starts at a
structure called the cisterna chyli (lumbar region) and receives lymph from the
entire left side of the body and from beneath the ribs on the right side of the
body. It returns lymph to the blood by emptying into the left subclavian vein.
The Right lymphatic duct receives lymph from
the right side of the body above the ribs and returns lymph into the right
subclavian vein. The entire route of fluid flow can be listed as follows:
Arteries (blood) → blood capillaries →
interstitial spaces (lymph) → lymphatic ducts → subclavian veins (blood).
Edema allows for greater
fluid to flow into lymphatic capillary.
Formation of Lymph
Fluid flows from
blood capillaries to form interstitial fluid. This fluid flows into the
lymphatic system and becomes lymph. Interstitial fluid contains
only a small amount of protein.
Lymphatic Tissue
Not all lymphatic
tissue is enclosed in a capsule. That not encapsulated is known as diffuse
lymphatic tissue and is found throughout the body. Examples include the lamina
propria of the GI tract, respiratory airways, urinary tract and reproductive
tract. Lymphatic nodules are oval shaped concentrations of lymphatic tissue. Tonsils are an example of lymphatic nodules.
The primary lymphatic organs are bone marrow and thymus gland. The bone marrow produces immunocompetent T & B cells. The thymus gland is where T-cells mature. Secondary lymphatic sites are lymph nodes and spleen. Most immune responses occur in the secondary lymphatic organs (nodes, nodules, and lymphatic tissue). Lymph nodes are oval or bean shaped and scattered throughout the body. They are usually found in clusters and covered by a capsule. Capsular extensions into the node are called trabeculae. The cortex or outer region of the node is packed with lymphocytes that are arranged in masses called follicles. The medulla or inner region of the node contains lymphocytes, macrophages and plasma cells. Flow into nodes via afferent lymphatic vessels and out via efferent lymphatic vessels. Efferent vessels emerge from the node at the hilum. The function of the node is to filter foreign materials from lymph (immune surveillance) and destroy filtered material by phagocytosis.
The tonsils are large aggregation of nodules in a mucous membrane. A single pharyngeal tonsil (also called adenoid) is found in posterior wall of nasopharynx. Paired palatine tonsils are the ones removed during a tonsillectomy. Paired lingual tonsils found at base of tongue. Function of the tonsils is to protect against foreign substances that are inhaled or ingested.
The spleen is the largest mass of lymphatic tissue in the body. Vessels enter and leave through a hilus. The spleen contains two types of tissue white pulp (mostly lymphocytes located around central arteries) and red pulp (venous sinuses filled with blood and cords of splenic tissue). The spleen does not filter lymph. Rather it functions as the site of B-cell proliferation into plasma cells, site of phagocytosis of bacteria and worn out RBC and platelets, and as a blood storage area.
The thymus gland is located in the superior mediastinum behind the sternum and between the lungs. It serves as a site for lymphocyte maturation into T-cells. After puberty it is composed mostly of fat and connective tissue.
Nonspecific Resistance to Disease
In general
resistance is the ability to fight off disease. Nonspecific resistance uses
defense mechanisms that fight off a wide range of pathogens whereas specific
resistance involves antibody formation against specific pathogen.
Physical, chemical, and barriers serve as the first line of defense. Skin and mucous Membranes provide a mechanical barrier that prevents microorganisms from penetrating sterile body compartments. The second line of defense, also nonspecific comes into play if organisms breech the first line. Components of the second line include interferon (protects against viral infections), the inflammatory response, fever, natural killer cells (special type of lymphocyte), and phagocytosis.
Specific Resistance to Disease
(Immunity)
In general immunity
is the ability of a body to defend against a specific invading agent such as
bacteria, toxins, virus and foreign tissue. Antigens are substances that provoke
the specific immune response. Properties that distinguish immunity from
non-specific defenses include specificity for a specific foreign molecule
(ability to distinguish self from non-self) and memory (subsequent responses
are more rapid and more intense).
Formation of T & B cells
Lymphocytes carry
out the immune responses. T and B-cells develop in the bone marrow. B-cells
mature in the bone marrow. T-cells migrate to the thymus gland where they mature
and become immunocompetent (the ability to carry out immune responses). Both
cell types acquire antigen receptors (proteins that recognize antigens). T-cells
develop into CD4 or CD8 cells by acquiring different proteins which allow for
different functions. In a cell-mediated immune
response, CD8 cells proliferate into Killer T-cells which directly attack cells
(invading antigen). Examples of invading antigens include intracellular
pathogens, fungi, parasites, viruses, some cancer cells and tissue transplants.
In antibody-mediated immune response,
B-cells transform into plasma cells and make antibodies (immunoglobulins). These
antibodies bind to and inactivate specific antigens. Antibodies work against
antigens found in body fluids, viruses, and extracellular pathogens such as
bacteria. Most CD4 T-cells become helper cells
that aid both CMI and AMI responses.
Antigens are a chemical substance that is recognized as foreign when it enters the body. The characteristics of an antigen are its ability to provoke a response (immunogenicity) and its ability to react specifically with the produced antibodies or cells (reactivity). Antigens are mostly proteins but they can be nucleoproteins, lipoproteins, or glycoproteins. A hapten (partial antigen) is a small substance that can elicit an immune response only when attached to a larger molecule.
For an immune response to occur, T and B-cells must recognize that a foreign antigen is present. The exogenous antigens are processed by antigen presenting cells (APC) that either ingest or bring the antigen into itself by endocytosis. There is a partial digestion the antigen, fusion of molecules within the APC, and finally the complex is released from the APC to combine with a B-cell. The B-cell is transformed into plasma cells that secrete antibodies into tissue or memory cells that can react with the antigen at later contact.
Antibodies combine with specific antigenic determinant that triggered its production. Antibodies consist of 2 heavy chains and two light chains. Within the chains are a variable portion (antigen binding site) and a constant portion (determines which class the antibody belongs too). The classes are IgA, IgG, IgM, IgE, and IgD. IgG is the only antibody that can cross the placenta (small), indicates a previous infection, comprises about 75% of all the antibodies in the body. IgM is the largest antibody, makes up 5-10% of antibodies in body, first antibody secreted after the initial exposure to any antigen, and indicates a current or recent infection. IgA antibodies offer local protection on mucous membranes. IgE antibodies are rare and are found in allergic reactions.
In cell-mediated immunity (CMI), there again is antigen recognition by T cells, proliferation of specific T-cells and differentiation into effector cells. The antigen is attacked and eliminated.
T-cells can differentiate into helper T-cells (have the CD4 protein, assist in CMI and AMI responses), killer T-cells (display the CD8 protein, kill foreign cells), suppressor T-cells, and memory T-cells (long lasting lymphocyte programmed to recognize the initial invader).
In antibody-mediated immunity B-cells differentiate into plasma cells which make antibody to specific antigen. This antibody is released into the circulation to reach the site of invasion. B-cells that don't differentiate into plasma cells remain as memory cells ready to respond to future invasions. B-cells can respond to unprocessed antigens, but their response is more intense when dendritic cells present antigen to them.
Immunological memory is the basis for immunization. Immunization against certain microbes is possible because of memory B and T-cells that remain after the primary response to an antigen. The secondary response provides protection much more rapidly should the same microbe enter the body again.
Types of Immunity and How Acquired
-
Naturally acquired active immunity: develop immune response by coming into contact with the antigen.
-
Naturally acquired passive immunity: transfer of IgG antibodies from mother to fetus across placenta or to newborn in mother's milk.
-
Artificially acquired active immunity: antibodies produced through vaccination.
-
Artificially acquired passive immunity: injection of antibodies (gamma globulin).
Self-Recognition and Immunological
Tolerance
T-cells undergo
+ selection to ensure that they can recognize self and that they do not
react to other self proteins (tolerance). Negative selection involves both
deletion and anergy which ensures that T-cells will not respond to fragments of
molecules that are present in the body. T-cells develop tolerance through
deletion (cells die) and anergy (cells become unresponsive to antibody
stimulation). The loss of immunological tolerance leads to autoimmune disease.
B-cells also develop tolerance through deletion and anergy.
Disorders of the immune system include overproduction of antibodies also called hypersensitivity reactions or underproduction of antibodies.
Hypersensitivity Reactions
-
Type I Classical immediate (anaphylaxis): hypersensitivity reaction to an antigen.
-
IgE’s react with exogenous antigens only in 30 minutes or less.
-
Due to histamine release and subsequent reactions. Atopic allergies (localized) depend on portal of entry such as Asthma, Hay fever, GI distress, and the Wheal & flare.
-
Anaphylaxis (generalized) requires antigen in blood: Small arteries dilate, decrease BP, circulatory failure. Bronchioles constrict causing asphyxiation. Reversal by adrenalin and antihistamines.
-
Type II = Cytotoxic
Circulating IgM and/or IgG from
B-lymphocytes that react in variable time frame. Transfusion reactions
(immediate). Autoimmune disease (longer). Erythroblastosis fetalis (longer).
Due to reaction of complement with antigens on specific
cells. Destruction of cells leads to cell debris & kidney damage.
Type III = Immune-complex mediated.
-
Circulating IgM and/or IgG from B-lymphocytes. React in 3-8 hours or longer.
-
Due to reaction of complement with antigens precipitating out. Acute Glomerulonephritis, some autoimmune diseases.
Type IV = Delayed hypersensitivity.
-
T-lymphocyte dependent. Reaction requires 24-72 hours. Direct destruction of cells by T-cells. Skin tests (TB), poison Ivy.
Immunodeficiency Disorders (ID)
ID can be primary immune deficiencies which are genetic in origin or secondary
immune deficiencies which are acquired. Among the primary ID are B-Cell defects
(Agammalobulinemia or Hypogammaglobulinemia), T-Cell defects (lack of all
classes of T cells), combined B-Cell and T-Cell defects (Severe combined
immunodeficiency disease, Adenosine deaminase deficiency), Phagocytic defects,
and complement defects.
Secondary immune deficiencies can result from natural causes such as diseases like AIDS or tuberculosis, stress, pregnancy, and aging. Acquired deficiencies can also result from immunosuppressive agents like irradiation, severe burns, steroids, and drugs that are used to treat graft rejection and cancer.
THE RESPIRATORY SYSTEM
Cellular metabolism requires O2 to produce energy. As a result of these reactions CO2 is produced. Excessive CO2 produces acidity which is toxic to cells and must be removed. Two systems supply O2 and remove CO2, the cardiovascular system and respiratory system. Failure of either system causes a disruption of homeostasis and rapid cell death due to O2 starvation and buildup of waste products.
Respiration is the exchange of gases between the atmosphere, blood and cells. Pulmonary ventilation (breathing) is the inspiration and expiration of air between the atmosphere and lungs. External (pulmonary) respiration is the exchange of gases between lungs and blood. Whereas internal (tissue) respiration is the exchange of gases between blood and cells.
The respiratory tract can be divided into the upper and lower tract. The upper respiratory tract contains the nose, pharynx (throat). The lower respiratory tract is comprised of the larynx, trachea, bronchi, and lungs. Except for some bones in the nose and pharynx, the skeleton of the respiratory tract is mostly cartilage down to the bronchioles where it is replaced by smooth muscle.
The conduction portion consists of all the structures that conduct air into and out of the lungs. Bronchial branches are numbered 0-16. Gases move by bulk flow from outside the body down through the terminal bronchioles. In the respiratory portion, branches 17-23, gas diffusion is the predominant process. It is here that the exchange of gases occurs in the alveoli and alveolar sacs.
Nose
The nasal cavity is
inside both the internal and external portion of the nose. A nasal septum
separates the nasal cavity into a left and right side. Three nasal conchae
(superior, middle and inferior) divide the nasal cavity into passageways (nasal
meatuses) that allow air to flow through. Incoming air is filtered, moistened
and warmed. Olfactory stimuli are received by receptors on olfactory epithelium
in the superior conchae. Hollow resonating chambers modify speech sounds. Mucous
membranes trap dust and with the aid of cilia move the debris to the throat for
elimination by swallowing or spitting.
Pharynx (Throat)
The pharynx starts at
the internal nares and ends at the cricoid cartilage. It lies posterior to oral
cavity, nasal cavity and larynx and is composed of the nasopharynx, oropharynx
and laryngopharynx. The pharynx functions in the passage of air, food and drink.
Larynx (Voice Box)
The
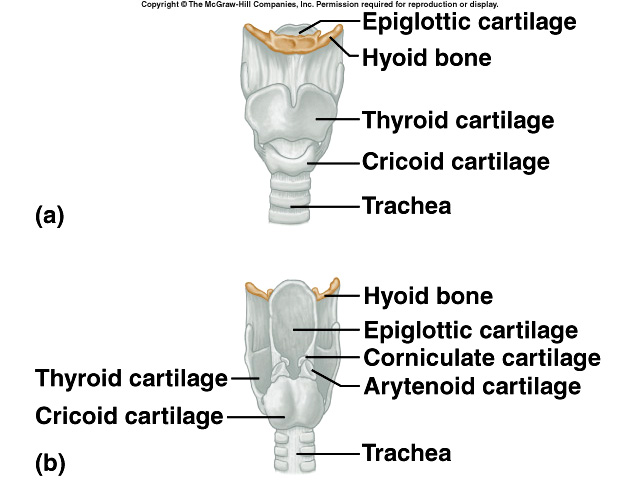 larynx
connects the laryngopharynx with the trachea. It is composed of pieces of
cartilage. The thyroid cartilage (Adam's apple) is the large piece that gives it
a triangular shape. The epiglottis is a leaf-shaped cartilage that closes to
prevent food and drink from entering the airway. Cricoid cartilage is a ring of
cartilage at the bottom of the larynx. Arytenoid cartilage is most important for
influencing vocal cords. Corniculate and cuneiform pairs of cartilage are also
present. Two pairs of folds extend inward from the laryngeal walls. The
ventricular folds are the upper pair and are called the false vocal cords
because they do not produce sounds. The space between them is called rima
vestibule. The vocal folds (lower pair) are the true vocal cords. The space
between is called rima glottides. Movement of vocal folds produces sound.
Tension and the length of the folds affect the pitch of sound.
larynx
connects the laryngopharynx with the trachea. It is composed of pieces of
cartilage. The thyroid cartilage (Adam's apple) is the large piece that gives it
a triangular shape. The epiglottis is a leaf-shaped cartilage that closes to
prevent food and drink from entering the airway. Cricoid cartilage is a ring of
cartilage at the bottom of the larynx. Arytenoid cartilage is most important for
influencing vocal cords. Corniculate and cuneiform pairs of cartilage are also
present. Two pairs of folds extend inward from the laryngeal walls. The
ventricular folds are the upper pair and are called the false vocal cords
because they do not produce sounds. The space between them is called rima
vestibule. The vocal folds (lower pair) are the true vocal cords. The space
between is called rima glottides. Movement of vocal folds produces sound.
Tension and the length of the folds affect the pitch of sound.
Trachea and Bronchi
The windpipe is a
passageway for air. It extends from the larynx to bronchi. The
trachea is shaped like incomplete rings or "C"
held together by trachealis muscle. The cartilage provides support. The open
part of "C" faces the esophagus, which allows the esophagus to expand into
trachea during swallowing. At the bronchi, there is an internal ridge called the
carina. The mucous membrane of the carina has a very sensitive mucous membrane
associated with a cough reflex.
The trachea branches into the right and left primary bronchi. The tracheobronchial tree consists of the trachea, primary bronchi (2) (to each lung), secondary bronchi (5) (to each lobe), tertiary bronchi (10) (to each bronchopulmonary segment), bronchioles and terminal bronchioles. They comprise the first 16 branches of the 23 total branches.
Lungs
The lungs are a pair
of cone-shaped organs that lie in the thoracic cavity. Gross anatomy reveals a
base, the bottom of lung that fits over diaphragm. The apex is the top point.
The costal surface lies against the ribs. The mediastinal surface contains the
hilum, an area through which bronchi, blood vessels, lymph vessels and nerves
enter and exit lung. The cardiac notch is an area in left lung where heart lies.
In the right lung there are three lobes (superior, middle, and inferior) and 2
fissures (horizontal and oblique). The left lung has only two lobes (superior
and inferior) separated by 1 fissure (oblique). Each bronchopulmonary segment
has many lobules that are wrapped in connective tissue that contains blood
vessels and lymphatic vessel. The terminal bronchioles divide into respiratory
bronchioles (branches 17-19) which divide into alveolar ducts (20-22). With each
generation of branching, cross-sectional area of airways increases such that by
the end there are @ 70-100 m2 of area for gas exchange in the lungs.
The alveolus is a cup shaped out pouching on the
alveolar ducts; there are @ 300 million alveoli 0.3 mm in diameter in each lung.
In the conduction portion of the lungs, the capillaries service the smooth
musculature. There are 250-300 billion in the lung or @ 1000 per alveoli
pulmonary capillaries. They are so interconnected they offer a sheet of blood to
the alveolar wall for gas exchange.
PHYSIOLOGY OF
RESPIRATION
The purpose of
respiration is to supply cells of the body with O2 and to remove
excess CO2. In pulmonary ventilation (breathing), gases are exchanged
between the atmosphere and alveoli as a result of differences in pressure
gradients. Air moves into the lungs by bulk flow when pressure inside the lungs
is less than atmospheric pressure and out when pressure is greater in the lung
than out in the atmosphere. For air to move into the lungs, the pressure inside
the lungs must decrease. Breathing or inspiration (inhalation) is achieved by
increasing the size of the lungs. The steps in lung expansion are:
-
contraction of the diaphragm and external intercostals;
-
contraction of diaphragm causes it to flatten, lowering its dome moving it 1-10 cm;
-
this accounts for @ 75% of air entering the lungs;
-
when intercostals contract, ribs are pulled upward & sternum is pushed forward.
Eupnea is normal quiet breathing, and includes shallow, deep or both. Costal breathing is shallow chest breathing, causing upward and outward movement of chest. Deep breathing is the outward movement of abdomen as a result of contraction and descent of diaphragm.
Expiration (exhalation) starts when inspiratory muscles relax. It is basically a passive process since muscles are relaxing and not contracting (does use some muscles with forced expiration). Factors involved include the recoil of elastic fibers that were stretched out during inspiration and the inward pull of surface tension due to film of alveolar fluid. Atelectasis (collapsed lung or a portion of the lung) is prevented by surfactant (substance released by Type II cells) which decreases surface tension. The maintenance of a low intrapleural pressure is vital to the functioning of the lungs.
Compliance is the ease with which the lungs and thoracic cavity walls expand. In high compliance the lungs easily expand. In low compliance the lungs resist expansion (“stiff” lungs, hard to inflate). Compliance is related to elasticity and surface tension. When conditions exist that destroy lung tissue (emphysema causes lungs to become filled with fluid; deficiency in surfactant; or impedance of lung expansion) a decrease in compliance is the result.
Airway resistance
Two factors must be overcome to move air into and out of the lung (elastic
forces and resistance, which is the most important factor). Some resistance is
found in airway walls chiefly at the medium sized bronchi. The least resistance
is found in terminal bronchiole. An increase in resistance is due to obstruction
(mucous, tumor, foreign bodies) and thus more pressure needed to get air into
lungs.
Pulmonary Air Volumes & Capacities (sum of > 2 volumes) aid in differentiating between two major types of lung disorders, obstructive and restrictive, and in quantifying the extent of the abnormality. They differ with ages, gender, and body type and are measured by using spirometer or respirometer.
-
tidal volume: 500 ml of air inspired or expired during a respiratory cycle;
-
anatomic dead space: that area that holds @ 150 ml of air that is not exchanged;
-
inspiratory reserve volume: @3000 ml, additional inspired air achieved by taking deep breath;
-
expiratory reserve volume: @1100 ml, additional expired air forced from lungs;
-
residual volume: 1200 ml: since lungs do not empty completely on exhalation, this is the air that remains in the non-collapsible air passages after maximal expiration;
-
minimal volume: tool used to determine whether or not infant was a stillborn;
-
Inspiratory capacity: 3500 ml, tidal volume and inspiratory reserve;
-
Functional reserve capacity: 2300 ml, resting volume of lungs, residual volume and expiratory reserve volume;
-
Vital capacity: 4600 ml is the maximum volume of air that can be exhaled after maximum inspiration and is the sum of inspiratory and expiratory reserve volumes and tidal volume;
-
Total capacity: 5800 ml, sum of all volumes or total volume of air in lungs when they are maximally inflated.
Obstructive disease: asthma
Narrowing of the airways due to a spasm of the smooth muscles, bronchial wall
edema or increased mucous production. Result is air is trapped in lungs.
-
á functional residual (reserve) capacity;
-
á residual volume;
-
á total lung capacity;
-
â vital capacity
Restrictive lung disease (pulmonary fibrosis) increase the ‘stiffness of the lung’ causing decreased lung compliance and increased lung recoil; the lungs cannot expand normally.
-
â vital capacity
-
â total lung capacity
-
â functional residual (reserve) capacity
-
â residual volume
Physiology of External
(Pulmonary) Respiration
External respiration (ER) is the exchange of O2
and CO2 between the alveoli of the lungs and the pulmonary
capillaries by diffusion. ER converts deoxygenated blood into oxygenated blood.
One factor involved is the partial pressure difference. Alveolar pO2
is higher than pO2 of systemic veins causing O2
to diffuse from alveoli into blood. A second factor is the surface area for gas
exchange. A decrease in the area of alveoli and there will be a decrease rate of
external respiration (emphysema). A third factor is the diffusion distances.
Normally it takes <1 second for O2/CO2 to cross the
membrane which is only 0.5um thick. Anything that increases the distance
(pneumonia) decreases rate of external respiration. Slowing of breathing rate or
shallowness of breath due to outside factors (drugs) can decrease rate of
external respiration.
Physiology of Internal
(Tissue) Respiration
Internal respiration
is the exchange of O2 and CO2 between tissue cells and
tissue capillaries. Blood returning to the heart is not fully oxygenated. Only
about 25% of available O2 enters tissue cells leaving a lot of O2
in the blood. Differences in the pressure gradients cause diffusion of O2
and CO2 between cells and capillary blood.
Transport of
Oxygen and Carbon Dioxide is a function of blood.
98.5% of oxygen is bound to hemoglobin in red blood cells. In 100 ml of
oxygenated blood there is 20 ml of O2. Each Hgb molecule has 4 heme groups which
can bind one molecule of O2. O2 + Hgb
D
HgbO2 (oxyhemoglobin). The pO2 is the most important factor that
determines how much O2 will combine with Hgb. As pO2
á more O2 combines with Hgb. In active tissues the pO2
of the tissue may â
to <40 mm Hg. This difference causes O2 in the blood to be released more easily
from blood to the tissue.
Hypoxia occurs when there is an O2 deficiency at the tissue level. Hypoxic hypoxia is low pO2 in arterial blood; results from higher altitude, obstruction of air passages or fluid in lung. Anemia hypoxia is too little Hgb in blood; results from hemorrhagic anemia or CO poisoning. Stagnant hypoxia is the inability of blood to carry O2 to tissue quickly enough; results from heart failure or circulatory shock. Histotoxic hypoxia occurs when O2 delivered but tissues prevented from using it; cyanide poisoning.
Carbon Dioxide
There are five ml CO2 in 100 ml of deoxygenated blood. CO2 is carried in three
forms: dissolved in plasma 7%, carbaminohemoglobin 23 %, and bicarbonate ions
70% transported in plasma.
Hgb + CO2 D HgbCO2 influenced by pCO2
CO2 + H2O D H2CO3 D H+ + HCO3-
carbonic anhyhrase carbonic acid bicarbonate
Summary of gas exchange in lungs and tissue
-
Deoxygenated blood returning to lungs containing
CO2 + HgbCO2 + HCO3- + H+ + H Hgb.
CO2 in plasma + carbaminohemoglobin + bicarbonate ions + buffering of H+ by Hgb -
The CO2 in the plasma diffuses into the alveoli & is exhaled.
-
The HgbCO2 splits; CO2 diffuses into alveoli and is exhaled.
-
The H+ + HCO3- combine to form H2O and CO2 which diffuses into the alveoli and is exhaled.
To maintain electrical balance as HCO3- declines in RBC and enters plasma, are exchanged for Cl- (chloride shift) as the Cl- ions move from the plasma into the RBC. CO2 diffuses out of RBC and is exhaled. At the same time O2 is being inhaled and diffusing from alveoli into RBC.
Control of Respiration
Nervous Control regulates the respiratory effort. Sensors detect the gases.
Messages are sent to the controllers in the
respiratory center. Effectors are the muscles that carry out respiration.
The respiratory center (in brain stem) is found in three areas. The medullary
rhythmycity area is in the medulla. It controls basic rhythm of respiration;
(inspiration @ 2 seconds, expiration @ 3 seconds). The pneumotaxic area in the
upper pons helps coordinate the transition between inspiration and expiration;
helps limit inspiration and facilitate expiration so that lungs don’t overfill
with air. The apneustic area in the lower pons receives impulses that prolong
inspiration and inhibit expiration when pneumotaxic area is inactive.
Regulation of Respiratory
center Activity
Cortical influences enable alteration of breathing, are protective so that we
don’t inhale gases or liquids, and make it impossible to kill self by holding
ones breath. The inflation reflex refers to stretch receptors in walls of
bronchi and bronchioles that when stimulated cause expiration. In chemical
regulation the goal is to maintain proper levels of CO2 and O2. Chemoreceptors
in blood (carotid and aortic bodies) sense changes in levels of CO2, O2 and H+.
Some definitions that are useful to know:
-
hypercapnia is an increase of pCO2 in the blood
-
hypocapnia is decrease in arterial pCO2
-
hyperventilation is a rapid and deep breathing (allows á level of CO2 to be expelled
-
hypoventilation is slow and shallow breathing
-
apnea is cessation of breathing
-
eupnea is normal breathing
Diseases of the
Respiratory System
(COPD) Chronic
obstructive Pulmonary Diseases
Asthma is a narrowing of the airways brought on by spasms of smooth
musculature in smaller bronchi and bronchioles. The patient has trouble exhaling
air is trapped in lungs. It is thought to be caused by hyper responsiveness to
specific and non-specific stimuli. Treatment for acute attacks requires the use
of epinephrine to help open airways. Inhaled corticosteroids are used in chronic
cases.
Bronchitis is inflammation of the bronchi where one gets mucous sputum production. Cigarette smoking is the leading cause of chronic bronchitis.
In emphysema the alveolar walls disintegrate leaving lungs filled with air during expiration. A key symptom is the reduced forced expiratory volume. It is caused by long term irritation such as smoking (most likely) or air pollution.
Lung Cancer starts in the walls of bronchi, but can spread throughout the body. It is caused by smoking and by inhalation of asbestos. Alveolar tissue that has been destroyed cannot be repaired. Surgery is performed in patients with localized disease. The majority initially thought to be “cured” usually succumb to metastatic disease.
Pneumonia is an acute infection in the alveoli of the lung. The alveolar sacs fill with fluid and dead WBC, blood pO2 decreased. Tuberculosis is a chronic wasting disease.
In Respiratory Distress Syndrome of the Newborn the alveoli collapse. It is thought to occur because of deficient amounts of surfactant in newborn’s alveoli. Mainly affects premature infants and treatment is limited.
In Respiratory failure the system cannot supply sufficient O2 to maintain metabolism or cannot eliminate CO2 to prevent respiratory acidosis. It always causes a dysfunction in other organs as well.
Coryza is the common cold caused by variety of viruses, mostly rhinovirus.
In Pulmonary embolism a clot in pulmonary artery obstructs blood flow to lung tissue can cause rapid death. The clot usually originates in deep veins of lower extremities.
Pulmonary Edema is an abnormal amount of interstitial fluid buildup in interstitial spaces and alveoli. It may occur with congestive heart failure.
Cystic Fibrosis is an inherited disease (genetic) linked to the ability to transport Cl- ions across the plasma membrane. Patients exhibit thick ropey secretions.
Smoke Inhalation Injury cause the inhibition of O2 delivery and utilization due to CO inhalation, upper airway injury due to heat, and lung damage from acids and aldehydes in smoke.





