
NERVOUS TISSUE
FUNCTIONS OF THE NERVOUS SYSTEM
The nervous system functions as a Sensory organ. Receptors sense changes within
and external to the body and pass that information to Integrative Centers that analyze the sensory
information, store data, and make decisions based on that data. Motor impulses
stimulate effectors to respond to the stimuli by initiating muscular
contractions or glandular secretions.
NERVOUS SYSTEM DIVISIONS
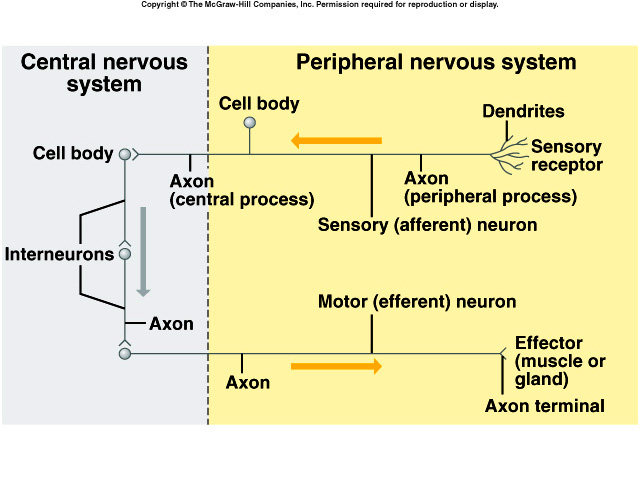
The nervous system contains the Central Nervous
System (CNS), the Peripheral Nervous System (PNS),
and the Autonomic nervous system. The CNS comprises the brain and spinal cord
and is connected to sensory receptors, muscles, glands by the peripheral nervous
system. Peripheral Nervous System (PNS) include cranial nerves that arise in the
brain and spinal nerves that arise in the spinal cord. Sensory or afferent
neurons in various parts of the body bring impulses into CNS. Motor or efferent
neurons send impulses from CNS to muscles and glands.
 The
PNS can be further subdivided into the Somatic nervous system (voluntary) and
the Autonomic nervous system (involuntary). In the somatic nervous system,
neurons conduct impulses from cutaneous and special sense receptors to the CNS
and motor neurons conduct impulses from CNS to skeletal muscle tissue. Since the
Autonomic nervous system is involuntary, sensory neurons from viscera send
impulses to CNS, and impulses from CNS are sent to smooth muscles, cardiac
muscles and glands.
The
PNS can be further subdivided into the Somatic nervous system (voluntary) and
the Autonomic nervous system (involuntary). In the somatic nervous system,
neurons conduct impulses from cutaneous and special sense receptors to the CNS
and motor neurons conduct impulses from CNS to skeletal muscle tissue. Since the
Autonomic nervous system is involuntary, sensory neurons from viscera send
impulses to CNS, and impulses from CNS are sent to smooth muscles, cardiac
muscles and glands.
HISTOLOGY OF NERVOUS TISSUE
Neurons differ
in structure and function. Based on structure, neurons are multipolar (several
dendrites and one axon), bipolar (one dendrite and one main axon), or unipolar
(one process extending from main body). Most neurons in brain and spinal cord
are multipolar. Unipolar neurons are always sensory. Bipolar neurons are found
in retina of eye, inner ear and olfactory area of brain. Based on direction or
function, neurons are sensory [(afferent) in which nerve impulses from receptors
are carried to the brain or the spinal cord], interneuron or association neurons
conduct impulses to other neurons (most neurons in body are this type and are
found exclusively in the CNS), or motor
(efferent) neurons [conduct impulses (effectors) from the brain or spinal cord
to effectors (muscles or glands)].
Most neurons have a cell body, many dendrites, and usually a single axon. Dendrites conduct impulses from receptors or other neurons to the cell body. The axon conducts impulses from the neuron to the dendrites or cell body of another neuron or to an effecter organ of the body at a synapse. The axon joins the cell body at the axon hillock. The first portion of the axon is the initial segment; where nerve impulses arise (trigger zone). Nerve fiber is a general term for any neuronal process (dendrite or axon). These processes of neurons are arranged into bundles called nerves in the PNS and tracts in the CNS. Nerve bodies in the PNS form clusters called ganglia. Axonal transport can be a fast or slow natural mechanism of intracellular transport in neurons.
CLASSIFICATION OF NEUROGLIAL CELLS
Neuroglia are
specialized tissue cells that support neurons, attach neurons to blood vessels,
produce the myelin sheath, and carry out phagocytosis. Neuroglia are found in
the CNS. Astrocytes participate in brain development and help form the
blood-brain barrier. Oligodendrocytes are the most common glia cells in CNS.
They produce the myelin sheath. Microglia protect the CNS by engulfing microbes.
Ependymal cells are epithelial cells that produce CSF and assist in its
circulation. The accepted theory has been that the neurons did all the
communicating in the brain and nervous system, and that the glial cells merely
nurtured the neurons. Recent research has demonstrated that glia cells
communicate with one another as well as with the neurons and that the glial
cells can alter the signals at the synaptic gaps. As a result, glial cells may
be critical in learning and memory functions.
Neuroglial cells found in the PNS include neurolemmocytes (Schwann cells) that produce myelin sheaths around neurons in the PNS. Satellite cells support neurons in PNS.
Myelination is the process by which a myelin sheath is produced around the axons in the CNS and PNS. Those axons that are sheathed are called myelinated, those axons that aren’t are called unmyelinated. The sheath electrically insulates the axon and increases the speed of the nerve impulse conduction
REGENERATION OF NERVOUS TISSUE
At about 6 months of age, neuronal cells lose their ability to divide. Once a
neuron is destroyed, it is permanently lost. Only some types of damage can be
repaired. In the PNS, damage to myelinated axons and dendrites may be repaired
if the cell body remains intact and if the neurolemmocytes remain active. In the
CNS, injury to the brain or spinal cord is usually permanent to the neural
cells.
NEUROPHYSIOLOGY
Cell membranes are usually charged or polarized. This means that there is an
unequal distribution of ions on either side of the membrane. Ions pass through
membranes via pores or protein channels. There are two types of channels, leakage (nongated)
and gated ion channels. Leakage channels are always open. Gated channels open
and close in response to some stimulus. Examples of gated channels include
voltage-gated, chemically gated, mechanically gated, and light-gated.
Voltage-gated ion channels in nerves and muscle plasma membranes give these
cells excitability. The presence of chemically, mechanically, or light-gated ion
channels in a membrane permits the appropriate stimulus to cause a graded
potential.
Resting Membrane Potential
A cell that is not being stimulated to send an impulse is in a resting state.
Factors that contribute to resting membrane potential include unequal
distribution of ions across the plasma membrane (high concentration of sodium
ions outside the cell and a high concentration of potassium inside), or a large
concentration of negatively charged ions inside the cell, and the relative
permeability of the plasma membrane to sodium and potassium. In a resting cell
more positive ions leave the cell than enter it.
Graded Potentials
Grades potentials are produced by the opening and closing of chemically gated
channels. The flow of ions through a particular channel may cause either
depolarization (polarization less negative than the resting level) or
hyperpolarization (more negative than the resting level), depending on the
charge of the ion and the direction of flow.
Action Potential (Impulse)
A sequence of events that results first in depolarization and then
repolarization is called action potential. Repolarization restores the resting
membrane potential and allows inactivated sodium channels to revert to their
resting state.
Refractory period
During the refractory period, another impulse cannot be generated at all
(absolute refractory period) or can only be triggered by a suprathreshold
stimulus (relative refractory period). An action potential conducts (propagates)
from point to point along the membrane. The traveling action potential is a
nerve impulse.
All-or-none principle
If a stimulus is strong enough to generate an action potential, the impulse
travels at a constant and maximum strength for the existing conditions. A
stronger stimulus will not cause a stronger impulse. All the impulses conducted
on a axon are the same.
Impulse conduction
A saltatory conduction occurs when the impulse jumps from neurofibral node to
another node. This phenomenon is more energy efficient and is used in quick
responses. A continuous conduction is a step-by-step depolarization of adjacent
areas. Propagation speed of a nerve impulse is not related to stimulus strength.
Larger diameter fibers conduct impulses faster than small ones. Myelinated
fibers conduct impulses faster than unmyelinated ones. Nerve fibers conduct
impulses faster when warmed and slower when cooled. The intensity of a stimulus
is coded in the rate of impulse production, i.e., the frequency of action
potentials.
Transmission at Synapses
A synapse is the functional unit between one neuron and another or between a
neuron and an effector such as a muscle or gland. At an electrical synapse,
ionic current spreads directly from one cell to another through gap junctions.
They are faster than chemical synapses, can synchronize the activity of a group
of neurons or muscle fibers, and may allow two way transmissions of impulses. At
a chemical synapse, there is only one-way information, transfer from a
presynaptic neuron to a postsynaptic neuron.
Neurotransmitters
Both excitatory and inhibitory neurotransmitters are present in the CNS and PNS.
The same neurotransmitter may be excitatory in some locations and inhibitory in
others. Examples of neurotransmitters are acetylcholine (Ach), glutamate,
aspartate, norepinephrine, epinephrine, and dopamine. Excitatory
neurotransmitter is one that can depolarize or make less negative the
postsynaptic neuron’s membrane. A depolarizing postsynaptic potential is called
an excitatory postsynaptic potential (EPSP). An inhibitory neurotransmitter
hyperpolarizes the membrane of the postsynaptic neuron, making the inside more
negative and generation of nerve impulse more difficult.
An inhibitory postsynaptic potential (IPSP) neurotransmitter is removed from the synaptic cleft in three ways, diffusion, enzymatic degradation, and uptake into cells and is necessary for normal synaptic function. Certain synapses can modify the quantity of neurotransmitter released at other synapses. Presynaptic facilitation increases the amount of neurotransmitter released by a presynaptic neuron whereas presynaptic inhibition decreases the amount. Both can last for several minutes to hours and may be important in learning and memory. If several presynaptic end bulbs release their neurotransmitters at about the same time, the combined effect may generate a nerve impulse due to summation. Summation may be spatial or temporal.
Disorders associated with neurotransmitter imbalance include Alzheimer’s disease, clinical depression, epilepsy, Huntington’s disease, Parkinson’s disease, Myasthenia gravis, Schizophrenia, and possibly SIDS.
Alteration of Impulse Conduction and
Synaptic Transmission
A neuron’s chemical and physical environment influences both impulse conduction
and synaptic transmission. Chemical synaptic transmission may be stimulated or
blocked by affecting neurotransmitter synthesis, release, removal, or the
receptor site. Alkalosis, acidosis, mechanical pressure and others may all
modify impulse conduction and/or synaptic transmission.
Neuronal Pools & Circuits
Neurons in the CNS are organized into different patterns called neuronal pools.
Each pool differs from all others and has its own role in regulating
homeostasis. A neuronal pool may contain thousands to millions of neurons.
Neuronal pools are organized into circuits which can be simple series,
diverging, converging, reverberating (oscillatory), or parallel after-discharge
circuits.
NERVE PATHWAYS (a route an impulse travels through the nervous system)
Reflex Arcs usually include a sensory neuron, a reflex center composed of
interneurons, and a motor neuron. They are the behavioral unit of the nervous
system. In Reflex Behavior, the reflexes are automatic, unconscious responses to
changes. They help maintain homeostasis. For example, knee-jerk employs only two
neurons and withdrawal reflexes are protective actions.
THE BRAIN & SPINAL CORD
THE MENINGES
The meninges are three coverings that run
continuously around the spinal cord and brain. The outermost layer is the dura
matter, the middle layer is the arachnoid, and the innermost layer is the pia
matter which contains many blood vessels.
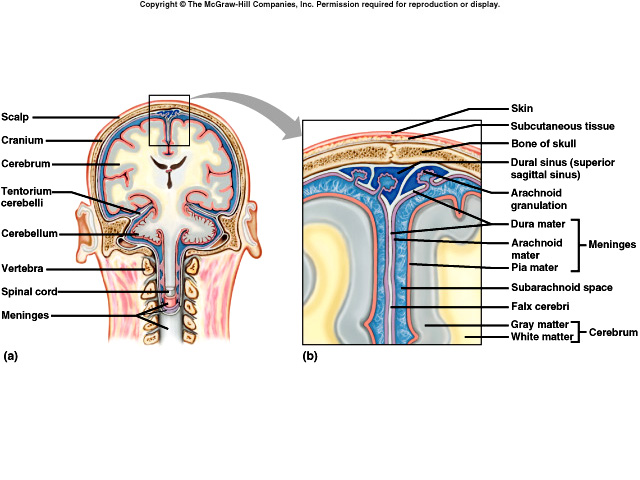 Between
the vertebral wall and dura matter is the epidural space which is lined with
fat, blood vessels, and connective tissue (protective layer). Between the dura
matter and the arachnoid is the subdural space which contains interstitial
fluid. Between the arachnoid and pia matter is the subarachnoid space which
contains cerebral spinal fluid. Inflammation of the meninges is called
meningitis and requires immediate clinical intervention.
Between
the vertebral wall and dura matter is the epidural space which is lined with
fat, blood vessels, and connective tissue (protective layer). Between the dura
matter and the arachnoid is the subdural space which contains interstitial
fluid. Between the arachnoid and pia matter is the subarachnoid space which
contains cerebral spinal fluid. Inflammation of the meninges is called
meningitis and requires immediate clinical intervention.
VENTRICLES AND CEREBRAL SPINAL FLUID (CSF)
Ventricles are interconnected cavities within the cerebral hemisphere and brain
stem and are filled with CSF. The choroid plexuses in the walls of the
ventricles secret CSF and it is reabsorbed into the blood through the arachnoid
villi. About 500 cc of CSF are secreted daily of which about 140 cc are
present at any one time. Most CSF is produced in the lateral ventricles. CSF
functions in mechanical protection (floating shock absorber), in chemical
protection by producing a stable ionic concentration, and in circulation for
exchange of nutrients and wastes.
SPINAL CORD ANATOMY
The spinal cord is protected by the vertebral
column. The meninges, cerebral spinal fluid, vertebral ligaments, and
denticulate ligaments protect the spinal cord against shock and displacement.
External Anatomy of the Spinal Cord
The spinal cord begins as a continuation of the
medulla oblongata and terminates at about the second sacral vertebra in an
adult. It is composed of thirty-one segments, each giving rise to a pair of
spinal nerves. It contains the cervical and lumbar enlargements that serve as
points of origin for nerves to the extremities. The tapered end of the spinal
cord is the conus medullaris, from which arise the filum terminale and cauda
equina. The spinal cord is divided into left and right sides by the anterior
medium fissure and posterior median sulcus. A spinal tap removes CSF to diagnose
pathologies and to administer drugs.
Internal
Anatomy of the Spinal Cord
The gray matter is shaped like the letter H and is surrounded by white matter;
gray matter is divided into horns and white matter into columns. White matter is
composed of bundles of myelinated nerve fibers. In the center of the spinal cord
is the central canal, which runs the length of the spinal cord and contains CSF.
Parts of the spinal fluid observed in cross section are the gray commissure,
central canal, anterior, posterior, and lateral gray horns, anterior, posterior
and lateral white columns, and ascending and descending tracts. The spinal cord
conveys sensory and motor information by way of the ascending and descending
tracts, respectively.
SPINAL CORD PHYSIOLOGY
Sensory and Motor Tracts
A major function of the spinal cord is to
convey nerve impulses from the periphery to the brain (via
sensory tracts) and to conduct motor impulses
from the brain to the periphery (via motor tracts).
Sensory information travels up the spinal cord to the brain along three main
routes on each side of the cord: the spinothalamic tracts and the posterior
column tracts (fasciculus gracilus and fasciculus cuneatus). The spinothalamic
tracts conduct impulses related to pain, temperature, touch and deep pressure.
Proprioception is awareness of movements of muscles, tendons, and joints.
Discriminative touch is the ability to feel exactly what part of the body is
touched. Two-point discrimination is the ability to feel when two points are
touched even if they are close together.
The descending tracts are corticospinal, reticulospinal, and rubrospinal tracts found in the lateral portions of the spinal cord. Motor information travels from the brain down the spinal cord to the muscles and glands along two main descending tracts, the pyramidal tracts (corticospinal tracts) and the extrapryamidal tracts (reticulospinal and rubrospinal tracts). The direct (pyramidal) tracts carry impulses for voluntary movements. The indirect (extrapyramidal) tracts carry impulses for automatic movements of voluntary muscles. Many of the fibers in the ascending and descending tracts cross over in the spinal cord or brain.
Reflexes
A second function of the spinal cord is to be an integrating center for spinal
reflexes: done in the gray matter. A reflex is a fast, predictable, automatic
response to changes in the environment that helps to maintain homeostasis.
Reflexes may be spinal, cranial, somatic, or autonomic. A reflex arc is the
simplest type of pathway; pathways are specific neuronal circuits and include at
least one synapse. The components of the reflex arc are the receptor, sensory
neuron, integrating center, motor neuron, and effector. Reflexes help the body
maintain homeostasis by permitting the body to make exceedingly rapid
adjustments to homeostatic imbalances. Somatic spinal reflexes include the
stretch (myostatic) reflex, reflex neuron, integrating center, motor neuron.
BRAIN
The brain is the largest and most complex part of the nervous system. It contains nerve centers that are associated with sensations. The brain issues motor commands and carries on higher mental functions.
Brain development
During embryonic development, brain vesicles or cavities (prosencephalon,
mesencephalon, and rhombencephalon) are formed from a neural tube, which serves
as forerunners of various parts of the brain. The forebrain develops into the
telencephalon and the diencephalons. The midbrain develops into the
metencephalon and the myelencephalon.
Five resulting cavities remain as ventricles in the mature brain. Ultimately the telencephalon develops into the cerebrum. The diencephalon develops into the epithalamus, thalamus, subthalamus, and hypothalamus, the mesencephalon develops into the midbrain, the metencephalon becomes the pons and cerebellum, and the myelencephalon becomes the medulla oblongata.
Hindbrain & Midbrain
BRAIN STEM
The brain stem extends from the base of the cerebrum to the spinal cord and
consists of the midbrain, pons, and medulla oblongata. The midbrain contains
reflex centers associated with eye and head movement. The pons transmits
impulses between the cerebrum and other parts of the nervous system, and
contains centers that help regulate the rate and depth of breathing. The medulla
oblongata transmits all ascending and descending impulses, and contains several
vital (heart rate, respiratory rate) and non-vital reflex centers. The reticular
formation regulates muscle tone; helps maintain consciousness and awakening from
sleep.
CERUBELLUM
The cerebellum consists of two hemispheres connected by the vermis. A thin
cortex surrounds the white matter of the cerebellum. The cerebellum functions
primarily as a reflex center, coordinating skeletal muscle movements and
maintaining equilibrium.
Forebrain
DIEENCEPHALON
The diencephalon begins where the midbrain ends and surrounds the third
ventricle. Found in the diencephalons are the epithalamus, thalamus, subthalamus, and
hypothalamus. The thalamus contains nuclei that that serve as relay stations for
all sensory impulses to the cerebral cortex, registers conscious recognition and
temperature, and plays a role in cognition and awareness. The hypothalamus
regulates the autonomic nervous system, secretes a variety of regulating
hormones, functions in rage and aggression, controls body temperature, regulates
food and fluid intake, and establishes a diurnal sleep pattern. Memory is
established in phases and is stored in both hemispheres utilizing the limbic
system, which is found in the central hemispheres, and the diencephalon. The
limbic system also functions in emotional aspects of behavior. The pineal gland
found in the epithalamus secrets melatonin which plays a role in sleep and
setting of the body’s biological clock.
Structure of the Cerebrum
The cerebrum can be described as two lobes of cerebral hemisphere connected by
the corpus callosum. Its surface is marked with ridges, grooves that increase
the surface area. A sulcus is a shallow groove. Separating the hemispheres is a
deep groove called a fissure. Covering the cerebral cortex is a thin layer of
gray matter, mostly composed of the neuron cell bodies. White matter is myelinated
and unmyelinated nerve fibers that interconnect neurons with the nervous system
and communicate with other body parts. The lobes are named after the skull
bones; (frontal, parietal, temporal, and occipital, insula).
Function of the cerebrum
The cerebrum carries out higher brain functions such as thought, reasoning,
interpretation of sensory impulses, control of voluntary muscles and memory
storage. The cerebral cortex has sensory, motor, and association areas. The
primary motor regions are found near the central sulcus in the frontal lobe.
Other areas include the motor speech area and special motor areas. Primary
sensory areas are found in the occipital area (sight), temporal area (sound),
frontal lobe (taste). Association areas analyze
and interpret sensory impulses and provide memory, reasoning, verbalizing,
judgment and emotions. One cerebral area dominates for certain intellectual
functions. Left hemisphere is important for right-handed control, spoken and
written language, numeric and scientific skills, and reasoning. Right
hemisphere is more important for left-handed control, musical and artistic
awareness, space and pattern perception, insight, imagination, and generating
images of sight, sound, touch, taste and smell.
Basal nuclei (Basal Ganglia)
These are masses of gray matter located deep within the cerebral hemispheres.
They relay motor impulses originating in the cerebral cortex, and aid in
controlling motor activities.
Peripheral Nervous System (PNS)
The peripheral nervous system consists of cranial and spinal nerves that branch out from the brain and spinal cord to all body parts. It is divided into the Somatic and the Autonomic Nervous Systems.
Cranial Nerves
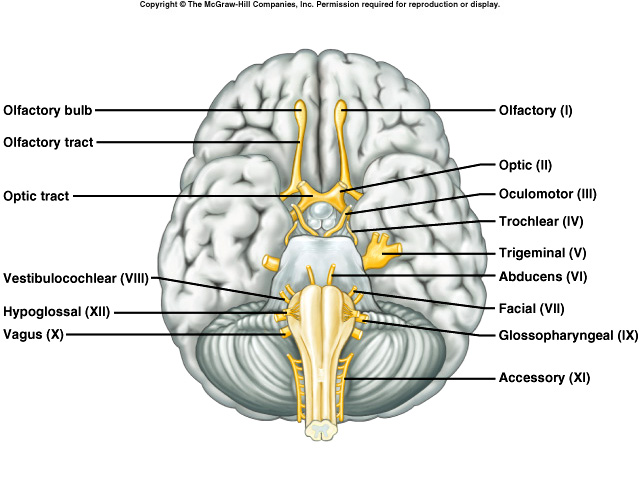 Twelve
pair of cranial nerves connects the brain to various body parts. Some are mixed,
some sensory, some are motor. Their names indicate either their distribution or
their function. They can either be somatic or autonomic.
Twelve
pair of cranial nerves connects the brain to various body parts. Some are mixed,
some sensory, some are motor. Their names indicate either their distribution or
their function. They can either be somatic or autonomic.
(I) Olfactory, (II) Optic, (III) Oculomotor, (IV) Trochlear, (V) Trigeminal (Opthalmic, Maxillary and Mandibular divisions, (VI) Abducens, (VII) Facial, (VIII) Vestibulocochlear, (IX) Glossopharyngeal, (X) Vagus, (XII) Accessory (Cranial and Spinal branches), (XII) Hypoglossal
Spinal
nerves
Thirty-one pair originate in the spinal cord and provide a two-way communication
system between the spinal cord and the arms, legs, neck and trunk. They are
grouped according to the vertebral levels from which they arise and are numbered
sequentially. They have dorsal and ventral roots. Dorsal roots contain sensory
fibers and have a dorsal root ganglion. Ventral roots contain motor fibers. Just
beyond its foramen, each spinal nerve divides into several branches. Most spinal
nerves form plexuses that direct nerve fibers to a particular body area.
AUTONOMIC SYSTEM
A key characteristic of the autonomic system is
that it functions without conscious effort, primarily controlling visceral
activities that maintain homeostasis. Autonomic functions are reflexes
controlled from the hypothalamus, brain stem, and spinal cord. It is divided
into the sympathetic and parasympathetic divisions.
Sympathetic division prepares the body for stressful and emergency
situations. Parasympathetic division is most
active under normal conditions. Sympathetic fibers leave the spinal cord and
synapse in specific ganglia. Parasympathetic fibers begin in the brain stem and
sacral region of the spinal cord and synapse in ganglia near various visceral
organs or in the organs themselves.
THE SPECIAL SENSES
RECEPTORS AND SENSATIONS
Each type of receptor is sensitive to a
distinct stimulus. Major types of receptors include chemoreceptor (sensitive to
changes in chemical concentration), pain receptors (sensitive to tissue damage),
thermoreceptor (sensitive to mechanical forces), photoreceptors (sensitive to
light), and mechanoreceptors (sensitive to mechanical forces such as changes in
pressure or movement of fluids).
Sensory impulses
When receptors are stimulated, changes occur in their membrane potentials.
Receptor potentials are transferred to nerve fibers triggering action
potentials. Sensations are feelings from sensory stimulation. A particular part
of the sensory cortex interprets every impulse that reaches it in the same way.
The cerebral cortex projects a sensation back to the region of stimulation.
Sensory adaptations are adjustments of sensory receptors to continuous
stimulation. Impulses are triggered at slower and slower rates.
OLFACTORY SENSATIONS: SMELL
The receptors for olfaction, which are bipolar
neurons, are in the nasal epithelium in the superior portion of the nasal
cavity. Substances to be smelled must be volatile, water-soluble, and
lipid-soluble. Adaptation to odors occurs quickly, and the threshold to smell is
low; only a few molecules of a substance need be present in air to be smelled.
Olfactory receptors convey nerve impulses to olfactory (I) nerves, olfactory
bulbs, olfactory tracts, and the cerebral cortex and limbic system.
GUSTATORY SENSATIONS: TASTE
The gustatory receptor cells are located in
taste buds. Substances to taste must be in solution in saliva. The four primary
tastes are sour (mainly on the side of the tongue), salty (tip of tongue),
bitter (back of tongue), and sweet (tip of tongue). The senses of smell and
taste are very closely related; impaired ability to smell significantly affects
one’s ability to taste. Think about the ability to taste food when you have an
upper respiratory tract infection. Adaptation to taste occurs quickly; the
threshold varies with the taste involved. Taste receptor cells convey nerve
impulses to cranial nerves V, VII, IX, and X, the medulla, the thalamus, and the
parietal lobe of the cerebral cortex.
AUDITORY SENSATIONS AND EQUILIBRIUM
External (outer) ear collects the sound waves
and passes them inwards. The outer ear consists of the auricle, external
auditory canal and tympanic membrane. Ceruminous glands secrete cerumen into the
external canal that helps prevent dust and foreign objects from entering the
ear.
Middle Ear (Tympanic cavity) is a small, air-filled cavity in the temporal bone that is lined by epithelium. The middle ear consists of auditory (Eustachian) tube, auditory ossicles (malleus, incus, and stapes), and the oval and round windows.
The Internal (inner) ear (labyrinth) contains two main divisions; an outer bony labyrinth that encloses an inner membranous labyrinth. The bony labyrinth is a series of cavities named on the basis of shape; semicircular canals and the vestibule (contain receptors for equilibrium), and the cochlea which contains receptors for hearing. The inner ear is lined with periosteum and contains a fluid called perilymph which is chemically similar to CSF. The fluid surrounds the membranous labyrinth. The membranous labyrinth is a series of sacs and tubes inside of and having the same general shape as the bony labyrinth. It is lined with epithelium and contains a fluid called endolymph, which is chemically similar to interstitial fluid.
The vestibule is the oval central portion containing two sacs: utricle and the saccule.
Semicircular canals and Cochlea
The anterior and posterior canals are oriented vertically and the lateral one is
oriented horizontally. One end of each canal enlarges into a swelling called an
ampulla. The portions of the membranous labyrinth that lie inside the
semicircular canals are called the semicircular ducts. The cochlea is divided
into three channels. The channel above the bony portion is the scala vestibuli,
which ends at the oval window. The channel below is the scala tympani, which
ends at the round window. Both contain perilymph. The third channel is the
cochlear duct (scala media). Membranes separate the cochlear duct from the other
two channels. Resting on the basilar membrane is the
spiral organ (Organ of Corti), the organ of hearing. Hair cells of the
spiral organ are easily damaged by continual exposure to high intensity sounds
and may degenerate, producing deafness. Projecting over and in contact with the
hair cells is the tectorial membrane, a delicate and flexible gelatinous
membrane.
Sound Waves result from alternate compression and decompression of air molecules. Normal range of hearing is between 1000 and 2000 Hertz (cycles/second). The frequency of a sound wave is its pitch; the greater the intensity (size) of the vibration, the louder the sound as measured in decibels.
Events of Hearing
The auricle directs the sound waves into the
external auditory canal. Sound waves strike the tympanic membrane, causing it to
vibrate back and forth. The vibration conducts from the tympanic membrane
through the ossicles. The malleus, connected to the eardrum, moves, causing the
incus and the stapes to move back and forth, pushing the membrane of the oval
window in and out. The movement of the oval window sets up fluid pressure waves
in the perilymph of the scala vestibuli. Pressure waves in the scala vestibuli
are transmitted to the scala tympani and eventually the round window, causing it
to bulge inward into the middle ear. As the pressure waves deform the walls of
the scala vestibuli and scala tympani, they push the vestibular membrane back
and forth causing increasing and decreasing pressure of the endolymph inside the
cochlear duct. The pressure fluctuations of the endolymph move the basilar
membrane slightly, moving the hair cells of the spiral organ against the
tectorial membrane; the bending of the hairs produces receptor potentials that
lead to the generation of nerve impulses in cochlear nerve fibers. Pressure
changes in the scala tympani cause the round window to bulge outward into the
middle ear.
Differences in pitch cause specific regions of the basilar membrane to vibrate more intensely than others. High-frequency sounds result in vibration near base of cochlea. Low-pitch sounds vibrate at apex of cochlea. Hair cells convert a mechanical force into an electrical signal; hair cells release a neurotransmitter, which initiates nerve impulses. Nerve impulses from the cochlear branch of the vestibulocochlear (VIII) nerve pass to the cochlear nuclei in the medulla. Most impulses then cross to the opposite side and then travel to the midbrain, to the thalamus, and finally to the auditory area of the temporal lobe of the cerebral cortex.
Physiology of equilibrium
Static equilibrium refers to the maintenance of
the position of the body (mainly the head) relative to the force of gravity. The
maculae of the utricle and the saccule are the receptors for equilibrium.
Dynamic equilibrium is the maintenance of body position (mainly the head) in
response to sudden movements, such as rotation, acceleration, and deceleration.
The cristae in the ampulla of the semicircular ducts are the primary sense
organs of dynamic equilibrium.
VISUAL SENSATIONS
Accessory Structures of the Eye include eyebrows, eyelids, eyelashes, lacrimal apparatus, and extrinsic eye muscles (superior, inferior, lateral and medial rectus and the superior and inferior oblique move the eyeballs, usually in concert with each other). The conjunctiva is a thin mucous membrane that lines the inner aspect of the eyelids and is reflected onto the anterior surface of the eyeball. The lacrimal apparatus consists of structures that produce and drain tears. “Watery” eyes occur when the normal drainage for the lacrimal glands is overwhelmed or obstructed. Tears contain lysozyme which has antibacterial properties.
Anatomy
of the Eyeball
The eye is composed of three layers. The
fibrous tunic is the outer coat of the eyeball: divided into posterior sclera
and anterior cornea. Junction of the sclera and cornea: opening known as the
scleral venous sinus or canal of Schlemm. The sclera, “white’ of the eye is a
white coat of dense fibrous tissue covers the entire eyeball except the most
anterior portion, gives the eyeball its shape, protects the inner parts. The
posterior area is pierced by the optic nerve (II). The cornea is a nonvascular,
transparent, fibrous coat through which the iris can be seen; acts in refraction
of light; contains many nerve fibers with low pain thresholds. Corneal
transplants are the most common organ transplant.
The vascular tunic is the middle layer and is composed of three portions; the choroid absorbs light rays so they are not reflected and scattered within the eyeball; it also provides nutrients to the posterior surface of the retina. The ciliary body consists of the ciliary processes and ciliary muscle. The processes consist of folds on the internal surface of the ciliary body where the epithelial lining cells secrete aqueous humor. The muscle is a smooth muscle that alters the shape of the lens for near or far vision. The iris is the colored portion seen through the cornea and consists of circular iris and radial iris smooth muscle fibers arranged to form a doughnut-shaped structure. The black hole in the center of the iris is the pupil, the area through which light enters the eyeball. The function of the iris is to regulate the amount of light entering the posterior cavity of the eyeball.
The third and inner coat is the retina (nervous tunic), lines the posterior three-quarters of the eyeball. Its primary function is image formation. It consists of a pigmented epithelium (nonvisual portion) and a neural portion (visual portion). The pigmented epithelium aids the choroid in absorbing stray light rays. The macula lutea is in the exact center of the posterior portion of the retina to the visual axis of the eye. The fovea centralis is found in a depression in the macula lutea.
The neural portion contains three zones of neurons: photoreceptor neuron, bipolar neurons, and ganglion neurons. Photoreceptor neurons are called rods or cones because of their outer segments. Rods are specialized for black-and-white vision in dim light: allow us to discriminate between different shades of dark and light and permit us to see shapes and movement. Cones are specialized for color vision and sharpness of vision in bright light; most densely concentrated in the central fovea, a small depression in the macula lutea. The fovea is the area of sharpest vision because of the high concentration of cones. Rods are absent from the fovea. A detached retina is often due to trauma of the head, but may be reattached by laser surgery.
The nonvascular lens is located just behind the pupil and the iris. Its function is to fine-tune light rays for clear vision. Loss of transparency is a cataract and is usually found with aging. The interior of the eyeball is a large space divided into two cavities by the lens: anterior cavity and posterior (vitreous) cavity. The anterior cavity is divided into anterior chamber and posterior chamber. The anterior cavity is filled with aqueous humor (AH) that is constantly being secreted by the ciliary processes behind the iris. The aqueous humor flows forward from the posterior chamber to the anterior chamber and drains into the scleral venous sinus and then into the blood. AH is replaced about every 90 minutes. Intraocular pressure is produced mainly by the aqueous humor. Excessive intraocular pressure is called glaucoma.
The posterior cavity (vitreous chamber) lies between the retina and the lens and is filled with a gel like substance called vitreous humor (VH). VH contributes to intraocular pressure, prevents the eyeball from collapsing, and holds the retina flush against the internal portions of the eyeball. VH is formed during embryonic development and is not replaced during life.
Image Formation
Image formation on the retina involves refraction of light rays by the cornea
and lens, accommodation of the lens, and constriction of the pupil. The bending
of light rays at the interface of two different media is called refraction; the
anterior and posterior surfaces of the cornea and of the lens refract entering
light rays so that they come into exact focus on the retina. Images are focused
upside-down and right to left reversal on the retina; the images undergo a
mirror reversal in the brain. Abnormalities of refraction are due to improper
shape of the eyeball or to irregularities in the surface of the lens or cornea.
Accommodation is an increase in the curvature of the lens, initiated by ciliary
muscle contraction, which allows the lens to focus on near objects. To focus on
far objects, the lens flattens out and the ciliary muscles relax. Constriction
of the pupil means narrowing the diameter of the hole through which light enters
the eye; this occurs simultaneously with accommodation of the lens and prevents
light rays from entering the eye through the periphery of the lens. In
convergence, the eyeballs move medially by action of the extrinsic eye muscles.
Physiology of Vision
The first step in vision transduction is the absorption of light by
photo-pigments on rods (@ 100 million) and cones (@ 3 million) which causes the
photopigments to decompose. Photopigments are colored proteins that undergo
structural changes upon light absorption.
The single type of photopigment in rods is rhodopsin. There are three types of photopigments in cones (RGB = red, green, blue). Bleaching and regeneration of the photopigments accounts for much but not all of the sensitivity change during light and dark adaptation. Once receptor potentials develop in rods and cones, they release neurotransmitters that induce graded potentials in bipolar cells and horizontal cells.
Visual Pathway
Horizontal cells transmit inhibitory signals to bipolar cells; bipolar or
amacrine cells transmit excitatory signals to ganglion cells, which depolarize
and initiate nerve impulses.
Impulses from ganglion cells are conveyed through the retina to the optic (II) nerve, through the optic chiasma and the optic tract, to the thalamus, and finally to the cortex (occipital lobes). Stereoscopic vision: perceives height, width, and depth of vision.
DISORDERS OF SPECIAL SENSES
Glaucoma is abnormally high intraocular
pressure, due to a buildup of aqueous humor inside the eyeball, which destroys
neurons of the retina. It is usually seen in the elderly. In cataracts the lens
becomes cloudy, opaque or yellow. Specks are floaters in the aqueous humor.
Deafness is significant or total hearing loss. Causes can be sensorineural (damage or destruction of nerve), conduction or mechanical. Otitis media refers to an acute infection of the middle ear, primarily by bacteria. Motion Sickness is a functional disorder precipitated by repetitive angular, linear, or vertical motion and characterized by nausea and vomiting. Preventative measures are more effective.
THE ENDOCRINE SYSTEM
ENDOCRINE GLANDS
The body contains two types of glands; exocrine
and endocrine glands. Exocrine glands (sudoriferous, sebaceous, and digestive)
secrete their products through ducts into body cavities or onto body surfaces.
Endocrine glands secrete their products (hormones) into extracellular spaces
around the secretary cell. The secretion diffuses into capillaries and is
carried away by the blood to a target tissue.
COMPARISON OF NERVOUS AND
ENDOCRINE SYSTEMS
Together the nervous and endocrine systems
coordinate all body systems. The nervous system controls through nerve impulses
conducted along axons of neurons. The endocrine system releases hormones which
are delivered to tissues throughout body by blood. Certain parts of the nervous
system stimulate or inhibit the release of hormones and hormones may promote or
inhibit nerve impulses. The nervous system causes muscular contraction or
glandular secretion, the endocrine system alters metabolic activities, regulates
growth and development, and guides the reproductive process. Nerve impulses are
generally much faster but the responses are briefer than hormones which are
slower in response timebut last longer.
HORMONES
Hormones only affect specific target cells that
have receptors to recognize a given hormone. Down-regulation occurs when the
number of receptors decreases, thereby decreasing the responsiveness of the
target cell. Up-regulation occurs when hormone is deficient and makes target
tissue more receptive.
Types of hormones
Circulating hormones (endocrine) are hormones that pass into the blood to act on
distant target cells, thus may linger for minutes or hours. Local hormones
usually are inactivated quickly. For example paracrines act on neighboring cells
and autocrines act on the same cell that secreted them.
Chemical classification
Most hormones are either steroids or nonsteroids. Steroids are lipids that are derived from cholesterol;
examples include the sex hormones and aldosterone.
Biogenic amines are very simple molecules derived from amino acids; examples
include the thyroid hormones (T3 & T4),
epinephrine and norepinephrine (catecholamines). Peptides (short chains of amino
acids) and proteins (long chains of amino acids) include
thyroid stimulating hormone, antidiuretic hormone, insulin, glucagon, human
growth hormone and others. Eicosanoids were recently discovered hormone and
include prostaglandins and leukotrienes. Water soluble hormones circulate in
free form in the blood; lipid-soluble steroid and thyroid hormones are carried
attached to transport proteins.
MECHANISMS OF HORMONE ACTION
The mechanism depends on both the hormone and
the target cell. (Insulin stimulates synthesis of glycogen in the liver and
synthesis of triglycerides in adipose tissue. Lipid-soluble hormones diffuse
through the cell membrane into a cell. In a target cell, the hormone binds to and
activates receptors within the cytosol or nucleus altering gene expression.
Water-soluble hormones activate plasma membrane receptors. First messenger is
hormone that activates receptor on plasma membrane which activates G-protein. A
second messenger relays the message inside of the cell. Cyclic AMP (cAMP) is the
best known second messenger.
Hormonal interactions depend on the hormone’s concentration, abundance of receptors, influences by other hormones. In a permissive effect, the action of some hormones requires recent stimulation by other hormones. In some cases there may be a synergistic effect or antagonistic effect.
Control of Hormone Secretion
Most hormones are released on short bursts, with little or no release between
busts. Regulation maintains homeostasis and prevents over or underproduction.
Hormone secretion is controlled by signals from the nervous system, by chemical
changes in the blood, and by other hormones. Most control is through negative
feedback systems.
HYPOTHALAMUS AND PITUITARY GLAND
The hypothalamus is the major integrating link
between the nervous and endocrine systems. The hypothalamus and the pituitary
gland regulate virtually all aspects of growth, development, metabolism, and
homeostasis.
Pituitary gland consists of an anterior pituitary gland and posterior pituitary gland. Hormones of the anterior pituitary gland are controlled by releasing or inhibiting hormones produced by the hypothalamus. There are five cell types; somatotrophs which produce human growth hormone (hGH), lactotrophs which produce prolactin (PRL), corticotrophs that secrete ACTH and melanocyte stimulating hormone, thyrotrophs secrete thyroid-stimulating hormone (TSH), and gonadotrophs secrete follicle-stimulating hormone (FSH) and leutinizing hormone (LH).
Hormones of Anterior Pituitary Gland
- GH (somatotropin) stimulates body growth, has many effects on metabolism and is controlled by growth hormone inhibiting hormone-somatostatin (GHIH) and growth hormone releasing hormone (GHRH). Disorders associated with improper levels of hGH are pituitary dwarfism, giantism and acromegaly.
- TSH regulates thyroid gland activities (T3 - T4 production) and is controlled by TRH (thyroid releasing hormone).
- FSH regulates activities of the ovaries and testes and is controlled by (GnRH) gonadotropin releasing hormone.
- LH regulates activities of the ovaries and testes and is controlled by (GnRH) gonadotropin releasing hormone.
- Prolactin (PRL) helps initiate milk secretion and is controlled by PIH (prolactin inhibitory hormone) and PRH (prolactin releasing hormone).
- Melanocyte-stimulating hormone increases skin pigmentation and is controlled by melanocyte-releasing hormone and melanocyte-inhibiting hormone.
- ACTH regulates activities of the adrenal cortex and is controlled by CRH (corticotrophin releasing hormone).
Posterior Pituitary Gland
The posterior pituitary gland does not
synthesize hormone, but it does store two hormones made in the hypothalamus.
Oxytocin (OT) stimulates contraction of the uterus and ejection of milk from the
breasts. OT secretion is controlled by uterine distention and nursing. Synthetic
OT is often given to induce labor.
The other hormone is Antidiuretic hormone (ADH). ADH stimulates water reabsorption by the kidneys and arteriolar constriction. The effect of ADH is to decrease urine volume and conserve body water. ADH is controlled by osmotic pressure of the blood. A disorder with secretion of ADH is Diabetes insipidus which is a result in a hyposecretion of ADH which causes excretion of large amounts of dilute urine.
THYROID GLAND
Thyroid gland consists of thyroid follicles
which secrete hormones T3 and T4 and parafollicular cells
which secrete calcitonin. Thyroid hormones are synthesized from iodine and
tyrosine. Thyroid hormones regulate the rate of metabolism, growth and
development, and the reactivity of the nervous system. Secretion is controlled
by the level of iodine in the thyroid gland. Cretinism, myxedema, Graves’
disease and goiter are disorders associated with the thyroid gland. Calcitonin
lowers the blood level of calcium. Secretion is controlled by calcium levels in
the blood.
PARATHYROID GLANDS
Parathyroid glands are embedded in the
posterior surfaces of the thyroid gland. They secrete parathyroid hormone (PTH)
which regulates the homeostasis of calcium and phosphate by increasing the blood
calcium level and decreasing blood phosphate level. Secretion is controlled by
blood calcium levels. Tetany and Osteitis fibrosa are disorders associated with
the parathyroid glands. Tetany results from a deficiency of calcium caused by
hypothyroidism. Osteitis fibrosa is characterized by demineralized, weakened,
and deformed bones resulting from hyperthyroidism.
ADRENAL GLANDS
The adrenal glands lie on top of each kidney
and consist of an outer cortex and an inner medulla. Complete loss of
adrenocortical hormones leads to death due to dehydration and electrolyte
imbalance within days to a week. In the Adrenal Cortex are the zona glomerulosa,
zona fasciculata, and zona reticularis. Cortical secretions include
mineralcorticoids, glucocorticoids and gonadalcorticoids. Mineralcorticoids (Aldosterone)
increase sodium and water reabsorption and decrease potassium reabsorption.
Secretion is controlled by the renin-angiotensin pathway and the blood levels of
potassium. Hypersecretion of aldosterone leads to muscular paralysis and
hypertension.
Glucocorticoids (cortisol) promote normal organic metabolism, help resist stress and serves as anti-inflammatory substance. Secretion is controlled by CRH and ACTH from the anterior pituitary. Disorders of glucocorticoids production include Addison’s disease (hyposecretion of glucocorticoids and aldosterone) and Cushing’s disease (hypersecretion of cortisol and cortisone).
Gonadalcorticoids secreted by the adrenal glands usually have minimal effects. Excessive production results in virilism.
Adrenal Medulla
The adrenal medulla consists of hormone-producing cells, called chromaffin
cells, which surround large blood-filled sinuses. Medullary secretions are
epinephrine and norepinephrine. Hormones are released under stress by direct
innervation from the autonomic nervous system and mimic sympathetic responses.
They help the body reduce stress but are not essential for life.
PANCREAS
The pancreas produces exocrine (for digestion)
and endocrine (hormones) secretions. Endocrine portion consists of pancreatic
islets (islets of Langerhans) which are divided into four types of cells. Alpha
cells secrete the hormone glucagon which increases blood glucose levels.
Secretion is stimulated by low blood glucose level. Beta cells secrete the
hormone insulin. Insulin decreases blood glucose levels and is stimulated by a
high blood glucose. Disorders associated with Beta cell endocrine hormone
secretion include diabetes mellitus and hyperinsulinism.
Delta cells secrete growth hormone inhibiting hormone (GHIH) which acts as a paracrine to inhibit the secretion of insulin and glucagon. F-cells secrete pancreatic polypeptide, which regulates the release of pancreatic digestive enzymes.
REPRODUCTIVE GLANDS
Ovaries produce estrogen and progesterone which
are related to development and maintenance of female sexual characteristics,
reproductive cycle, pregnancy, lactation and normal reproductive functions.
Produce also inhibin and relaxin. These will be covered in extensively in the
reproductive unit. Testes produce testosterone which are related to development
and maintenance of male sexual characteristics and normal reproductive
functions. Also produced is inhibin.
PINEAL GLAND
Attached to roof of third ventricle inside the
brain is the pineal gland. It consists of pinealocytes, neuroglial cells and
post ganglionic sympathetic fibers. The pineal gland secretes melatonin in a
diurnal rhythm linked to the dark-light cycle. Seasonal affective disorder (SAD)
is thought to be due to over-production of melatonin.
THYMUS GLAND AND DIGESTIVE GLANDS WILL BE COVERED LATER.
Hyposecretion and Hypersecretion
Inadequate release of hormones from the endocrine glands results in
imbalances in the homeostasis which leads to disease. Too little hormone being
released is known as hyposecretion whereas too much hormone released is called
hypersecretion. The following table is a partial list of endocrine glands and
the disease states that occur in hypo- and hypersectrtion.
| Gland | Hormone | Hyposecretion | Hypersecretion |
| Pituitary | HGH | Pituitary dwarfism | Giantism |
| ADH | Diabetes insipidus |
***** |
|
| Thyroid | TSH | Cretinism (in infants) or Myxedema (in adults) | Graves disease |
| Adrenal | Cortisol |
***** |
Cushing's disease |
| Pancreas | Insulin | Diabetes mellitis |
***** |
STRESS AND THE GENERAL ADAPTATION
SYNDROME
Homeostatic mechanisms attempt to counteract the everyday stresses of living. If
successful, the body maintains normal limits of chemistry, temperature and
pressure. If stress is extreme, unusual, or long-lasting, these mechanisms may
not be sufficient, which triggers the general adaptation syndrome. Stressors are
the stimuli that produce the general adaptation syndrome. Include heat, cold,
operations, poisons, infections, fever, and strong emotional responses.
Stressors stimulate the hypothalamus via an immediate alarm reaction. They are
slower to start, but longer lasting, resistance reaction.
Alarm Reaction
This alarm reaction is also called the fight-or-flight reaction that increases
circulation, promotes catabolism for energy production, and decrease
nonessential activities.
Resistance reaction is initiated by regulating hormones of the hypothalamus (CRH, GHRH, and TRH). They are long term reactions and accelerate catabolism for energy to counteract stress. Exhaustion can result from changes during alarm and resistance reactions. If stress causing exhaustion is too great, it may lead to death.
Stress and disease
Stress can lead to diseases such as gastritis, ulcerative colitis, irritable
bowel syndrome, peptic ulcers, hypertension, asthma, rheumatoid arthritis,
migraine headaches, anxiety and depression. One can also develop a chronic
disease or dying prematurely if stressors are not reduced.





